Parasomnias
What they are, who they affect, their distinct types, and which treatments can help
If you’ve ever talked in your sleep, sleepwalked, or woken up with your heart racing after a frightening dream, you’ve experienced a parasomnia. Parasomnias are undesirable experiences that happen while a person is sleeping, falling asleep, or waking up . Most people experience parasomnias at some point in life.
In most cases, parasomnias are not harmful. But, they may be disturbing or frustrating. In some cases, parasomnia activity can be dangerous to sleepers or their bed partners, or a symptom of an underlying medical condition.
What Causes Parasomnias?
Not all parasomnias have a clear cause, but researchers have identified several potential causes and triggers for parasomnias.
- Sleep deprivation: If you don’t get enough sleep, you’re more likely to experience parasomnias . This may be because sleep deprivation can alter the stages of sleep .
- Disturbed sleep: Frequent nighttime sleep disruptions can provoke parasomnias. If you have a condition that disturbs sleep, such as sleep apnea, restless legs syndrome, or chronic pain, you may be more vulnerable to parasomnias.
- Stress: If you are feeling stress or anxiety, or if a negative life event has recently affected you, you may experience parasomnias .
- Psychological disorders: Research has linked depression, post-traumatic stress disorder (PTSD), and other mental health conditions to parasomnias.
- Neurological disorders and diseases: Conditions that affect the nervous system can cause parasomnias. These include narcolepsy, multiple sclerosis, Parkinson’s disease, dementia, brain tumors, and more.
- Medications: Some medications may make parasomnias more likely, including certain antidepressants.
- Inherited traits: Genes play a role in some parasomnias, so if you have a family history of a certain parasomnia, you may be more likely to experience them.
Is Your Troubled Sleep a Health Risk?
A variety of issues can cause problems sleeping. Answer three questions to understand if it’s a concern you should worry about.
Parasomnias and the Sleep Cycle
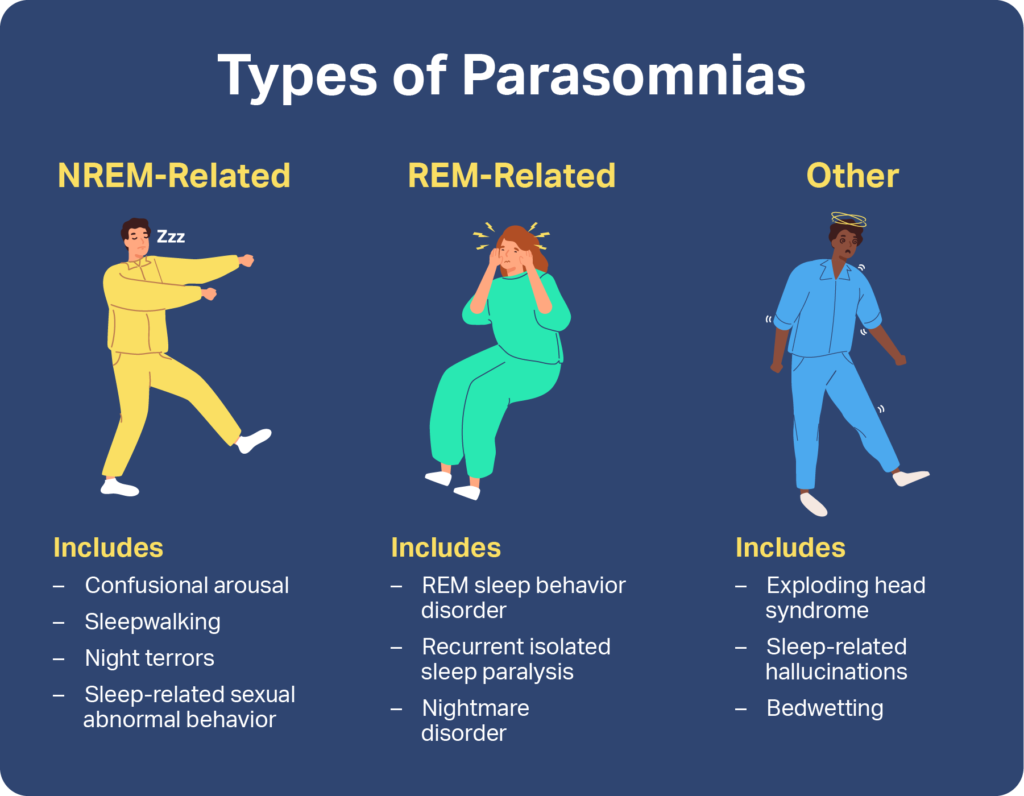
Sleep experts classify parasomnias by the stages of sleep they occur during. Some are associated with non-rapid eye movement (NREM) sleep, which encompasses the first three stages of sleep, while others happen during rapid eye movement (REM) sleep. Other parasomnias may occur during any sleep stage or during the transition into or out of wakefulness.
NREM-Related Parasomnias
The parasomnias that happen during NREM sleep are often described as “disorders of arousal.” People who experience them partially wake up. Their eyes may be open, and they may appear to act with intention. However, they may not respond when spoken to, and they may have no memory of what happened afterward . NREM-related parasomnias tend to be more common in children .
Night Terrors
People with night terrors abruptly wake from sleep feeling afraid, usually within a few hours of going to bed . Episodes often begin with a sleeper sitting up or bolting out of bed and screaming. They may breathe rapidly, sweat, and experience a racing heart and enlarged pupils. Efforts to calm or console someone in the midst of a night terror may not work.
While people can experience night terrors at any age, they are one of the most prevalent parasomnias of early childhood, affecting about 40% of children between the ages of 2 and 6 . Episodes can last anywhere from a few minutes to over half an hour. Unlike nightmares, people generally do not remember night terrors, though they can upset caregivers and bed partners.
Sleepwalking
Sleepwalking is a parasomnia that causes people to get out of bed and perform complex and seemingly purposeful behaviors, even though they aren’t awake . People who sleepwalk may get dressed, use the bathroom, prepare food, or even do housework.
Generally, sleepwalking happens in the first third of the night during N3 sleep, also known as deep sleep. Sleepwalking is more common in children, perhaps because children spend more time in deep sleep. Sleepwalking has been estimated to occur in about 15% of children ages 2 to 6 and 6% of children ages 6 to 11. In some cases, sleepwalking persists beyond childhood.
Sleepwalking can be dangerous. People have wandered outside on snowy nights, tripped or fallen, and driven cars while sleepwalking. If you or someone in your household sleepwalks, consider blocking stairs and closing windows before bedtime for safety.
Sleep-related Eating Disorder
People with sleep-related eating disorder (SRED) have recurring sleepwalking episodes in which they eat or drink. During these episodes, they may consume items like dog food, raw meat, frozen foods, cigarettes, or even cleaning products. In addition to the dangers posed by these behaviors, SERD can affect people’s health by causing weight gain and increasing their risk for high blood pressure, diabetes, and sleep apnea.
Confusional Arousals
During confusional arousals, sleepers wake in a state of extreme confusion. They may sit up, rub their eyes, or look bewildered. They may also cry, moan, or mumble. Confusional arousals typically occur within three hours of bedtime, but they can also happen when a caregiver or partner attempts to wake someone up. Episodes usually resolve within 15 minutes. About 17% of children and between 2% and 4% of adults experience confusional arousals.
Sleep-Related Abnormal Sexual Behaviors
Sleep-related abnormal sexual behaviors are a type of confusional arousals. People with this parasomnia, also called sexsomnia, engage in sexual activities without awareness of what they are doing. Often, they cannot recall what they did the next morning. While most confusional arousals are harmless, people with sleep-related abnormal sexual behaviors may unknowingly engage in violent or criminal sexual acts.

REM-Related Parasomnias
REM-related parasomnias occur during rapid eye movement (REM) sleep or in the transition out of it. These parasomnias tend to occur in the final hours of a night’s sleep, often very early in the morning. Unlike non-REM parasomnias, individuals can usually remember these episodes.
Nightmares and Nightmare Disorder
Nightmares are bad dreams that cause sleepers to wake up feeling anxious and upset. In contrast with night terrors, people usually recall nightmares in detail. Although they can occur any time, nightmares usually happen during REM sleep and in the last few hours of the night. Stress and trauma are known to provoke nightmares.
Nightmares affect about 50% of children and a majority of adults. While for most people, nightmares are occasional occurrences, about 20% of children and between 2% and 6% of adults have frequent nightmares. They may be diagnosed with a condition called nightmare disorder if their nightmares negatively affect their mental health, relationships, or ability to function.
REM Sleep Behavior Disorder
People with REM sleep behavior disorder (RBD) physically act out their dreams. They may gesture, kick, or punch while talking, screaming, or moaning. While some people sleep through mild RBD episodes, most wake up and recall their dreams.
RBD affects less than 1.5% of people . RBD is strongly associated with neurodegenerative diseases. When it occurs in children and young adults, it may be the result of narcolepsy or antidepressant use. Because RBD can cause people to fall out of bed or injure themselves or their bed partners, it’s important for people with this parasomnia to take steps to secure their sleeping environments in ways advised by a doctor.
Sleep Paralysis
During sleep paralysis, a person wakes to find themselves unable to move or speak . They may feel terror and dread or have visual, auditory, or sensory hallucinations. Between 7% and 15% of adults report having experienced sleep paralysis at least once. While episodes tend to be isolated events, some individuals who experience this phenomenon as children or teenagers have recurring episodes in adulthood .
Other Parasomnias
Some parasomnias are not associated with NREM or REM sleep, because they can happen at any time during sleep or they happen when a person is falling asleep or waking up. Sleep experts classify these behaviors and events as “other parasomnias.”
Bedwetting
While bedwetting is normal for young children, it is considered a parasomnia when it happens at least twice a week in people over age 5. In individuals who have never learned to hold their urine at night, this parasomnia likely has a genetic component. If bedwetting begins after a person has learned to control their bladder during sleep, a psychological trigger or sleep disorder may be to blame .
Exploding Head Syndrome
People with exploding head syndrome hear a sudden loud noise, often accompanied by a flash of light, as they are falling asleep or waking up . While these events are neither painful nor harmful, they can be distressing. Some people with this parasomnia experience “exploding head” events often, while for others, episodes are rare.
Sleep-related Hallucinations
Some people see, hear, or feel things that aren’t actually there as they fall asleep or wake up. Similar to sleep paralysis, sleep-related hallucinations can involve REM sleep intruding into wakefulness. Sleep hallucinations are strongly associated with narcolepsy .
Sleep-related Dissociative Disorders
Sleep-related dissociative disorders affect individuals in the moments after they have fallen asleep or awoken. These disorders cause episodes in which a person experiences disruptions in one or more of the following :
- Consciousness
- Sense of self or identity
- Mood
- Memory
- Control or perception of one’s body
During such episodes, which may last from a few minutes to over an hour, a person may scream, flail, cry, arch their backs, or act violently. They may have no memory of the event afterward. These parasomnias are strongly associated with a history of trauma and with certain psychiatric disorders .
How Are Parasomnias Treated?
Treatment for parasomnias can vary depending on the type of parasomnia and its cause. Some parasomnias require no treatment, while doctors may recommend managing others with:
- Healthy sleep habits
- Stopping or stopping certain medications
- Therapy
- Relaxation techniques
If you or someone in your care is experiencing parasomnias, talk to a doctor. A medical professional can help you manage symptoms, improve sleep, and stay safe throughout the night.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
17 Sources
-
Alshahrani, S. M., Albrahim, R. A., Abukhlaled, J. K., Aloufi, L. H., & Aldharman, S. S. (2023). Parasomnias and associated factors among university students: A cross-sectional study in Saudi Arabia. Cureus, 15(11), e48722.
https://pubmed.ncbi.nlm.nih.gov/38094542 -
Singh, S., Kaur, H., Singh, S., & Khawaja, I. (2018). Parasomnias: A comprehensive review. Cureus, 10(12), e3807.
https://pubmed.ncbi.nlm.nih.gov/30868021/ -
Kirsch, D. (2023, July 25). Stages and architecture of normal sleep. UpToDate.
https://www.uptodate.com/contents/stages-and-architecture-of-normal-sleep -
Vaughn, B. V. (2024, June 11). Approach to abnormal movements and behaviors during sleep. UpToDate.
https://www.uptodate.com/contents/approach-to-abnormal-movements-and-behaviors-during-sleep -
Zak, R., & Karippot, A. (2023, October 18). Nightmares and nightmare disorder in adults. UpToDate.
https://www.uptodate.com/contents/nightmares-and-nightmare-disorder-in-adults -
A.D.A.M. Medical Encyclopedia [Internet]. (2023, April 28). Night terrors in children. MedlinePlus.
https://medlineplus.gov/ency/article/000809.htm -
Mainieri, G., Loddo, G., & Provini, F. (2021). Disorders of arousal: A chronobiological perspective. Clocks & Sleep, 3(1), 53–65.
https://pubmed.ncbi.nlm.nih.gov/33494408/ -
Foldvary-Schaefer, N. (2023, September 7). Disorders of arousal from non-rapid eye movement sleep in adults. UpToDate.
https://www.uptodate.com/contents/disorders-of-arousal-from-non-rapid-eye-movement-sleep-in-adults -
Morse, A. M., & Kotagal, S. (2023, October 13). Parasomnias of childhood, including sleepwalking. UpToDate.
https://www.uptodate.com/contents/parasomnias-of-childhood-including-sleepwalking -
A.D.A.M. Medical Encyclopedia [Internet]. (2023, April 29). Sleepwalking. MedlinePlus.
https://medlineplus.gov/ency/article/000808.htm -
Howell, M., & Schenck, C. H. (2024, April 26). Rapid eye movement sleep behavior disorder. UpToDate
https://www.uptodate.com/contents/rapid-eye-movement-sleep-behavior-disorder -
A.D.A.M. Medical Encyclopedia [Internet]. (2023, April 20). Sleep Paralysis. MedlinePlus.
https://medlineplus.gov/ency/article/000801.htm -
Farooq, M., & Anjum, F. (2023, September 4). Sleep paralysis. StatPearls [Internet].
https://www.ncbi.nlm.nih.gov/books/NBK562322/ -
A.D.A.M. Medical Encyclopedia [Internet]. (2024, February 17). Bedwetting. MedlinePlus.
https://medlineplus.gov/ency/patientinstructions/000703.htm -
Khan, I., & Slowik, J. M. (2022, December 12). Exploding head syndrome. StatPearls [Internet].
https://www.ncbi.nlm.nih.gov/books/NBK560817/ -
Pelak, V. S. (2024, May 30). Approach to the patient with visual hallucinations. UpToDate.
https://www.uptodate.com/contents/approach-to-the-patient-with-visual-hallucinations -
Foote, B. (2024, May 23). Dissociative identity disorder: Epidemiology, pathogenesis, clinical manifestations, course, assessment, and diagnosis. UpToDate.
https://www.uptodate.com/contents/dissociative-identity-disorder-epidemiology-pathogenesis-clinical-manifestations-course-assessment-and-diagnosis













