How Sleep Works: Understanding the Science of Sleep
An introduction to the key details about what happens to the mind and body during sleep
Even after decades of research, the exact reason why we sleep remains one of the most enduring and intriguing mysteries in health science. To try to get to the bottom of this question, experts analyze how sleep works and what happens when we don’t get enough sleep.
Studies demonstrate that sleep is incredibly complex and has effects on virtually all systems of the body. Multiple parts of the brain are involved in the processes of producing hormones and chemicals that regulate sleep and wakefulness.
While there is much that is still to be learned about the intricacies of how sleep works, existing research sheds light on the mechanics of what happens in the brain and body during sleep. This knowledge reveals how sleep is connected to numerous elements of physical, emotional, and mental health and provides insights about how people can get better sleep.
What Happens When You Sleep?
Within a minute after falling asleep, notable changes start to affect both the brain and body. Body temperature drops, brain activity ramps down, and heart rate and respiration slow as well. Not surprisingly, the body’s energy expenditure is lower during sleep .
It is important to recognize, though, that what happens during sleep is dynamic. Over the course of one night, you actually progress through multiple sleep cycles, each of which lasts between 70 and 120 minutes and is composed of separate sleep stages. These sleep stages are fundamental to how sleep works.
What Are the Sleep Stages?
There are four stages of sleep divided into two categories. The first three stages fall into the category of non-REM (rapid eye movement) sleep. The fourth stage is REM sleep.
| Category of Sleep | Sleep Stage | Other Names | Normal Length |
|---|---|---|---|
| NREM | Stage 1 | N1 | 1-5 minutes |
| NREM | Stage 2 | N2 | 10-60 minutes |
| NREM | Stage 3 | N3, Slow-Wave Sleep (SWS), Delta Sleep, Deep Sleep | 20-40 minutes |
| REM | Stage 4 | REM Sleep | 10-60 minutes |
In stage 1, you’ve just dozed off and started transitioning to stage 2, which involves further slowing of activity in the brain and body. It’s much easier to be awoken during these early stages of the sleep cycle.
Stage 3 is the deepest part of NREM sleep. In this stage, your muscles and body relax even more, and brain waves show a clear pattern of slowed activity that is markedly different from waking brain activity. It is believed that deep sleep plays an important role in recuperation of the body as well as effective thinking and memory.
Stage 4 is the only stage of REM sleep. During this time, brain activity picks up significantly, and most of the body — except the eyes and breathing muscles — experience temporary paralysis. Although dreams can happen during any stage, the most intense dreaming takes place during REM sleep.
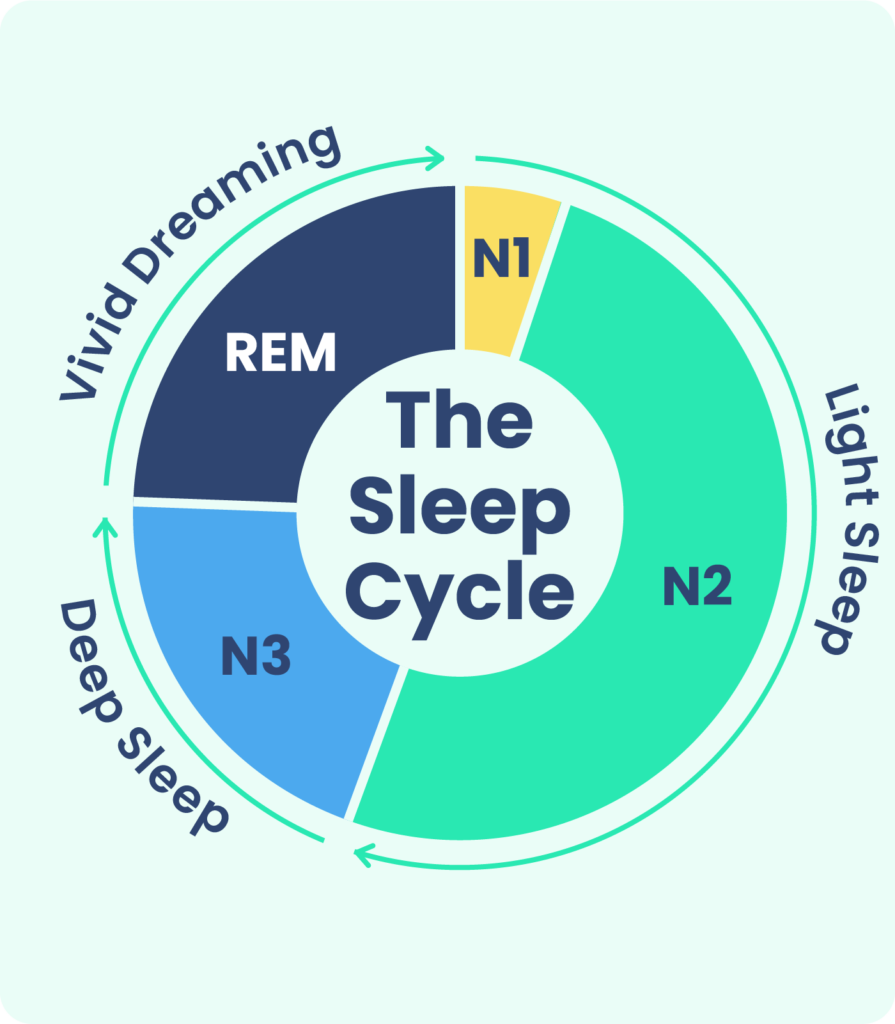
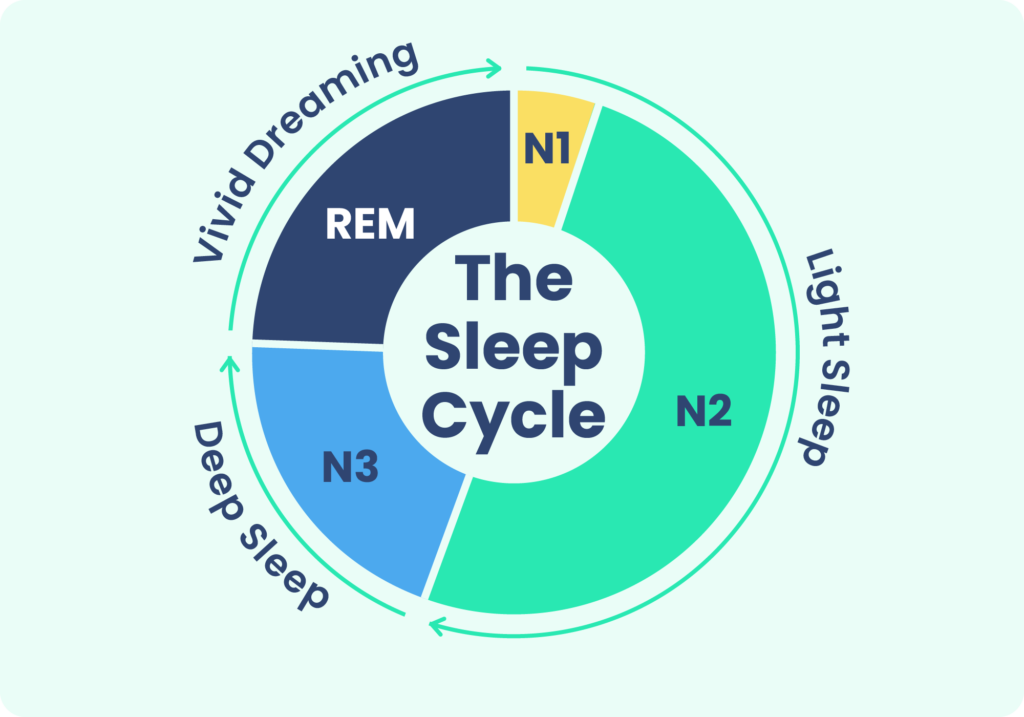
The REM sleep stage is believed to be essential for the brain, enabling key functions like memory and learning. As the night goes on, it’s normal to spend a greater percentage of time in REM sleep with most of it occurring in the second half of the night.
The structure of a person’s sleep stages and cycles is known as their sleep architecture. While deep sleep and REM sleep involve more profound changes in activity levels, experts believe that each stage plays a part in a healthy sleep architecture that generates quality sleep.

How Does the Body Regulate Sleep?
The body regulates sleep with two key drivers: sleep-wake homeostasis and the circadian alerting system.
- Sleep-wake homeostasis. This technical term describes something most of us know implicitly from experience: the longer you’re awake, the more you feel a need to sleep. This is because of the homeostatic sleep drive , the body’s self-regulating system in which pressure to sleep builds up based on how long you’ve been awake. This same drive causes you to sleep longer or more deeply after a period of insufficient sleep.
- The circadian alerting system. Part of your body’s biological clock, circadian rhythms last roughly 24 hours and play a central role in numerous biological processes, including sleep. Light exposure is the biggest influence on circadian rhythms, encouraging wakefulness during the day and sleepiness at night.
These two factors directly affect how much your body feels a need for sleep, reflecting your biological clock, the time of day, your light exposure, and how long you’ve been awake.
In addition, a wide range of external factors can influence sleep-wake homeostasis and the circadian alerting system. For example, stress or hunger may disrupt your normal process for sleep regulation. Caffeine intake or exposure to light from electronic devices are other examples of how behavioral choices can alter the body’s underlying systems for managing sleep.
These multifaceted processes are managed by several parts of the brain including the hypothalamus, the thalamus, the pineal gland, the basal forebrain, the midbrain, the brain stem, the amygdala, and the cerebral cortex. The fact that so many parts of the brain are involved in wakefulness and sleep, including the sleep stages, is further demonstration of the biological complexity of sleep.
What Chemicals and Hormones Regulate Sleep?
Numerous chemicals and hormones are involved in the mechanics of sleep-wake homeostasis and the circadian alerting system. Shifting between wakefulness and sleep creates changes in thousands of neurons in the brain and a complex signaling system that generates specific reactions in the body.
To date, there is much that is still unknown about the intricate processes that control sleep, but researchers have discovered some substances that appear to be important cogs in the machinery of sleep.
A chemical called adenosine is believed to play a central role in sleep-wake homeostasis. Adenosine builds up when we’re awake and appears to increase sleep pressure. Caffeine, on the other hand, suppresses adenosine, which may explain part of how it promotes wakefulness.
Neurotransmitters are chemicals that send signals within the nervous system to activate or deactivate certain cells. Examples of neurotransmitters involved in promoting wakefulness or sleep include GABA, acetylcholine, orexin, and serotonin.
Hormones also play an integral role in signaling and regulating sleep-wake states. Melatonin, which promotes sleep and is naturally produced as light exposure decreases, is one of the best known hormones related to sleep. Other important sleep-related hormones include adrenaline, cortisol, and norepinephrine. Sleep can also affect the production of vital hormones , such as growth hormone as well as leptin and ghrelin that regulate appetite, which may exert influence on sleep-wake homeostasis and circadian rhythms.
The function of these chemicals and hormones may be different in some individuals based on their genetics, which is why certain sleep disorders like sleep apnea may run in families. Environment and lifestyle choices may also influence the chemical and hormonal signaling responsible for sleep.
Why Is Sleep Important?
While even experts haven’t reached a consensus explanation for why we sleep, numerous indicators support the view that it serves an essential biological function.
From an evolutionary perspective, the fact that sleep exists in almost all animal species — despite the fact that it creates vulnerability and takes time away from feeding or procreating — is a strong indication that it is fundamental to well-being .
In humans, sleep appears to be critical to both physical and mental development in babies, children, and young adults. In adults, a lack of sleep has been associated with a wide range of negative health consequences including cardiovascular problems , a weakened immune system , higher risk of obesity and type II diabetes , impaired thinking and memory, and mental health problems like depression and anxiety.
These diverse ramifications of sleep deprivation offer strong support to the view that sleep doesn’t have just one biological purpose but in fact, through its complexity, is an important contributor to the proper functioning of nearly all of the systems of the body.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
9 Sources
-
Jung, C. M., Melanson, E. L., Frydendall, E. J., Perreault, L., Eckel, R. H., & Wright, K. P. (2011). Energy expenditure during sleep, sleep deprivation and sleep following sleep deprivation in adult humans. The Journal of physiology, 589(Pt 1), 235–244.
https://pubmed.ncbi.nlm.nih.gov/21059762/ -
Liu, S., Liu, Q., Tabuchi, M., & Wu, M. N. (2016). Sleep Drive Is Encoded by Neural Plastic Changes in a Dedicated Circuit. Cell, 165(6), 1347–1360.
https://pubmed.ncbi.nlm.nih.gov/27212237/ -
Saper, C. B., Fuller, P. M., Pedersen, N. P., Lu, J., & Scammell, T. E. (2010). Sleep state switching. Neuron, 68(6), 1023–1042.
https://pubmed.ncbi.nlm.nih.gov/21172606/ -
Kim, T. W., Jeong, J. H., & Hong, S. C. (2015). The impact of sleep and circadian disturbance on hormones and metabolism. International journal of endocrinology, 2015, 591729
https://pubmed.ncbi.nlm.nih.gov/25861266/ -
Schwartz, W. J., & Klerman, E. B. (2019). Circadian Neurobiology and the Physiologic Regulation of Sleep and Wakefulness. Neurologic clinics, 37(3), 475–486.
https://pubmed.ncbi.nlm.nih.gov/31256784/ -
Dahl R. E. (2007). Sleep and the developing brain. Sleep, 30(9), 1079–1080.
https://pubmed.ncbi.nlm.nih.gov/17910377/ -
Miller, M. A., & Cappuccio, F. P. (2007). Inflammation, sleep, obesity and cardiovascular disease. Current vascular pharmacology, 5(2), 93–102.
http://www.eurekaselect.com/openurl/content.php?genre=article&issn=1570-1611&volume=5&issue=2&spage=93 -
Del Gallo, F., Opp, M. R., & Imeri, L. (2014). The reciprocal link between sleep and immune responses. Archives italiennes de biologie, 152(2-3), 93–102.
http://www.architalbiol.org/index.php/aib/article/view/15293 -
Cappuccio, F. P., D’Elia, L., Strazzullo, P., & Miller, M. A. (2010). Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep, 33(5), 585–592.
https://www.ncbi.nlm.nih.gov/pubmed/20469800