5 Ways to Get More REM Sleep
For centuries, scientists believed sleep was simply a period of rest and relaxation. It was not until researchers discovered REM sleep in 1953 that experts realized sleep might be an active and complex process. Since then, sleep science has blossomed and researchers have found REM sleep to be important for several mental processes, including memory and learning .
We’ll discuss why REM sleep is essential and how to get more REM sleep if you are not getting enough.
Why Is REM Sleep Important?
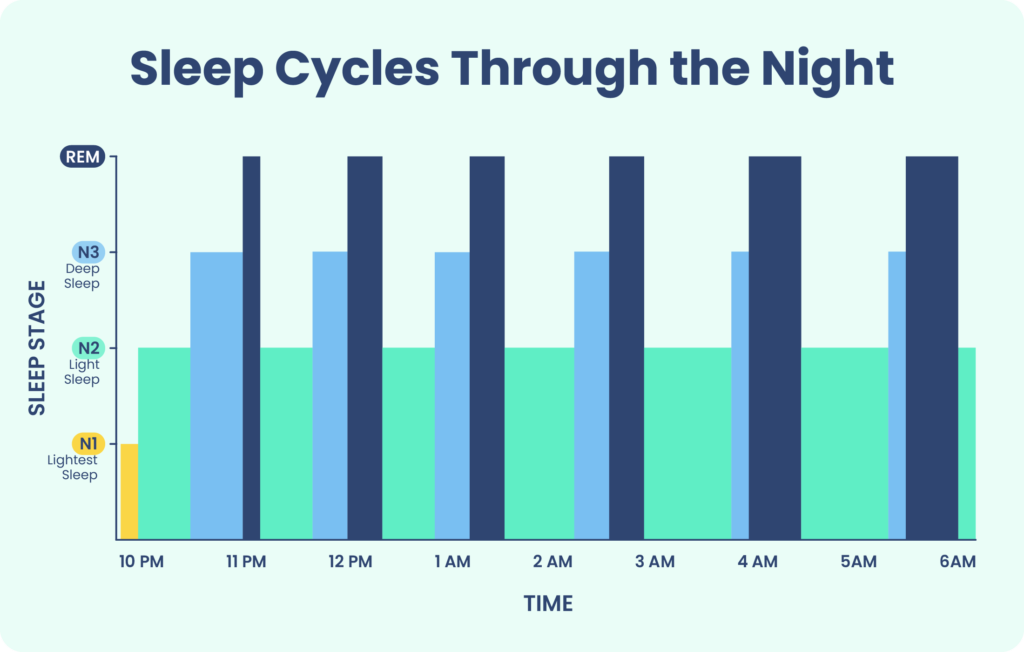
REM, a sleep stage characterized by rapid eye movement, is one of four sleep stages that we experience each night. The other three stages are referred to as non rapid eye movement sleep (NREM), because the eyes are mostly still during these stages. The average person experiences four to six REM episodes during a normal night of sleep.
REM sleep is the sleep stage commonly associated with dreaming. During this stage, the eyes move rapidly behind closed eyelids, and brain activity consists of smaller, faster waves, called theta waves, that are similar to wakefulness. Most muscles become temporarily paralyzed during REM sleep to prevent accidental harm from acting out dreams, although individuals may display occasional muscle twitches.
Are You Getting Enough REM Sleep?
A variety of issues can cause degrade your sleep quality. Answer three questions to understand if it’s a concern you should worry about.
Experts have found evidence suggesting REM sleep is a crucial part of memory consolidation and helps prepare and maintain neural connections to enhance future learning. Studies show that taking a nap and reaching the REM sleep stage leads to improvements in working memory .
Along the same lines, REM sleep likely plays a role in brain development, and the muscle twitches experienced during this sleep stage may contribute to motor learning. The sleep period of newborn babies consists of 50% REM sleep, lending support to the theory that REM sleep is important for the developing brain.
REM also appears to foster emotional processing and creativity . Although people can dream during both REM and NREM sleep, dreams during REM sleep are often more vivid and unusual, whereas dreams during NREM sleep are more grounded in reality. Other research has found that REM sleep may help people recover from stressful events, and obtaining larger amounts of REM sleep after a traumatic event may reduce the chances of developing post-traumatic stress disorder .
How to Get More REM Sleep
Since REM sleep occurs mostly during the second half of the sleep period, sleeping for too short a period may not allow time to complete all the REM sleep cycles. Thus, most recommendations for obtaining more REM sleep center around ensuring you are obtaining a sufficient quantity and quality of sleep.
Develop and Maintain a Sleep Schedule
For better sleep, it is important to go to bed and wake up at the same time every day , even on the weekends. Longer periods of REM sleep tend to align with the dip in body temperature that occurs in the early morning hours, which is regulated by the circadian rhythm. Disrupting this balance by keeping irregular sleep-wake times may confuse the body and interfere with REM sleep regulation.
Treat Sleep Disorders
If alterations in REM sleep are due to disruptions caused by a sleep disorder, then treating the disorder can prompt a return to normal proportions of REM sleep. For example, studies have found that after treating obstructive sleep apnea with continuous positive airway pressure (CPAP) therapy, people experience REM rebound sleep accompanied by better mood and higher-quality sleep overall. Your doctor or a sleep specialist can help you develop an appropriate treatment plan depending on your personal situation.

Stop Taking Sleep Aids
Certain antidepressant and antipsychotic medications may reduce or almost entirely suppress REM sleep, and cause REM rebound when people stop taking them. Many people take these medications for long periods of time and find the benefits are worth the drawbacks. However, if the lack of REM sleep is affecting your quality of life, ask your doctor if there are options for switching to another medication or lowering your dose.
Avoid Alcohol, Caffeine, and Tobacco
Drinking a moderate to high amount of alcohol can delay when you first enter REM sleep, and it can also cause you to spend less time in REM sleep overall. Caffeine and tobacco may also interfere with normal progression through the sleep stages, especially if these are consumed in the evening or close to your desired sleep period. Try to cut down on these substances and avoid them entirely in the late afternoon or evening.
Use Sleep Hygiene Techniques
Amounts of REM sleep usually stabilize once a person starts receiving quality sleep on a regular basis. Some experts recommend adopting sleep hygiene habits to improve sleep quality. Examples of sleep hygiene habits include:
- Exercising regularly
- Maintaining a cool, dark, and quiet bedroom environment
- Establishing a regular bedtime routine with soothing activities, such as reading or taking a warm bath
- Keeping gadgets and screens out of the bedroom
- If unable to sleep after 20 minutes, leaving your bed and doing something else in another room until you feel sleepy enough to return to bed
Sleep hygiene may be helpful for some people, but it is not considered sufficient treatment for people who have a diagnosed sleep disorder (such as insomnia) or other medical condition.
How Much REM Sleep Do You Need?
Adults need at least seven hours of sleep every night. REM sleep should make up around 20% to 25% of a person’s total time asleep. That said, experts usually give recommendations for overall sleep time rather than for REM sleep in particular, as the body tends to self-regulate to maintain a balanced level of sleep stages.
Going a little short on sleep might not have significant effects on REM sleep, but after 12 to 24 hours of sleep deprivation, people experience a REM rebound effect the next time they sleep. This term refers to an increase in REM sleep to make up for previously missed REM sleep.
What Can Upset REM Sleep?
REM sleep timing depends mostly on the circadian rhythm, the body clock that synchronizes processes such as body temperature and the sleep-wake cycle. The circadian rhythm is responsible for promoting REM sleep at certain times during the sleep period. By contrast, the total amount of REM sleep is regulated homeostatically, meaning the body seeks to obtain a set amount of REM sleep and compensates by spending more or less time in REM sleep if levels fall outside of this range.
Certain underlying conditions can affect the length and quality of REM sleep. For example, in people with depression, the first REM cycle occurs earlier in the sleep period and lasts longer. By contrast, people with insomnia tend to obtain less REM sleep. Antidepressant medications can suppress REM sleep , though scientists are working to understand why this reduction in REM causes seemingly little to no negative effects.
Disorders such as obstructive sleep apnea may cause interruptions in sleep that reduce the amount of time spent in REM sleep. Other sleep disorders directly affect REM sleep quality. For example, individuals with REM sleep behavior disorder do not experience the usual muscle paralysis during REM sleep, leaving them free to act out their dreams and potentially injure themselves . People with narcolepsy can fall asleep suddenly and go straight into REM sleep, at the cost of less deep sleep.
When to Talk to Your Doctor
Make an appointment with a medical professional if you are experiencing sleep problems or daytime symptoms such as excessive tiredness. Consider keeping a sleep diary in the days leading up to your visit to provide a clearer picture of your symptoms.
Sleep issues may be due to an undiagnosed medical condition or sleep disorder, which your doctor can help you treat. The body has ways of recuperating the lost REM sleep once the underlying condition is resolved, but it is important to address sleep problems once you notice them to prevent long-term health complications.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
11 Sources
-
Peever, J., & Fuller, P. M. (2016). Neuroscience: A distributed neural network controls REM sleep. Current Biology: CB, 26(1), R34–R35.
https://pubmed.ncbi.nlm.nih.gov/26766231/ -
Patel, A. K., Reddy V., Araujo J. F. (2019, March). Physiology, sleep stages. StatPearls.
https://pubmed.ncbi.nlm.nih.gov/30252388/ -
Lau, E. Y., Wong, M. L., Lau, K. N., Hui, F. W., & Tseng, C. H. (2015). Rapid-eye-movement-sleep (REM) associated enhancement of working memory performance after a daytime nap. PloS One, 10(5), e0125752.
https://pubmed.ncbi.nlm.nih.gov/25970511/ -
Malinowski, J. E., & Horton, C. L. (2021). Dreams reflect nocturnal cognitive processes: Early-night dreams are more continuous with waking life, and late-night dreams are more emotional and hyperassociative. Consciousness and Cognition, 88, Article 103071.
https://pubmed.ncbi.nlm.nih.gov/33360822/ -
Flaherty A. W. (2011). Brain illness and creativity: Mechanisms and treatment risks. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 56(3), 132–143.
https://pubmed.ncbi.nlm.nih.gov/21443820/ -
Feriante, J., & Singh, S. (2021). REM rebound effect. In StatPearls. StatPearls Publishing.
https://pubmed.ncbi.nlm.nih.gov/32809548/ -
Merck Manuals. Sleep hygiene. Merck Manual Professional Version.
https://www.merckmanuals.com/professional/multimedia/table/v41413035 -
Ebrahim, I. O., Shapiro, C. M., Williams, A. J., & Fenwick, P. B. (2013). Alcohol and sleep I: Effects on normal sleep. Alcoholism, Clinical and Experimental Research, 37(4), 539–549.
https://pubmed.ncbi.nlm.nih.gov/23347102/ -
Schwab, R.J. (2020, June). Overview of sleep. Merck Manual Professional Version.
https://www.msdmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
McCarthy, A., Wafford, K., Shanks, E., Ligocki, M., Edgar, D. M., & Dijk, D. J. (2016). REM sleep homeostasis in the absence of REM sleep: Effects of antidepressants. Neuropharmacology, 108, 415–425.
https://pubmed.ncbi.nlm.nih.gov/27150557/ -
American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders — Third Edition (ICSD-3) (Online).
https://aasm.org/








