Best Sleeping Position for Sleep Apnea
- Side sleeping can reduce snoring and improve other symptoms of obstructive sleep apnea.
- Back sleeping increases the risk of airways obstructions and can worsen sleep apnea symptoms.
- In any sleep position, it is best to elevate your head and align your neck and spine.
A person’s sleep position can have direct impacts on comfort, pain, and sleep quality. Sleep position can also affect sleep apnea. In general, experts identify side sleeping as the best position for sleep apnea and back sleeping as the worst.
Sleep position can play a role in both types of sleep apnea. Obstructive sleep apnea (OSA) occurs when a narrowed or blocked airway interferes with breathing repeatedly during sleep. Central sleep apnea (CSA) arises when the brain fails to send the signals required for the body to breathe normally.
Both OSA and CSA can be linked to people sleeping on their back. In fact, some research shows that more than half of people with OSA experience more severe symptoms when they sleep on their back.
By changing sleeping positions, many people can decrease their symptoms of OSA and CSA. We walk through the effects of side, stomach, and back sleeping positions on sleep apnea. We also discuss strategies for changing sleep positions, recommendations for head positioning, and additional options for sleep apnea treatment.
Sleeping on Your Side
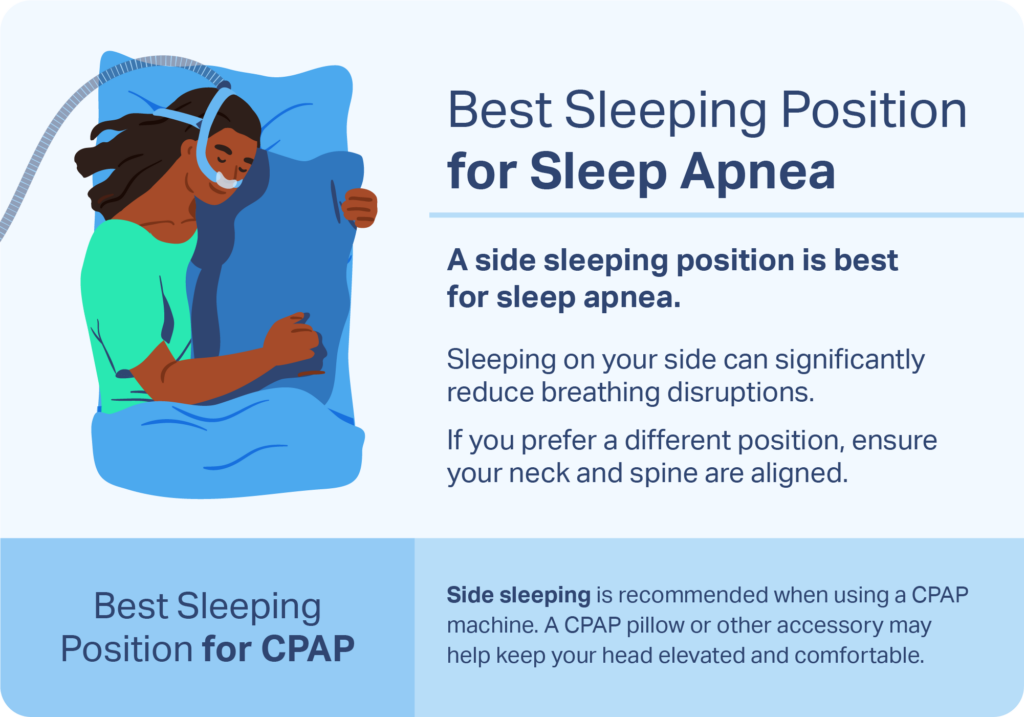
Side sleeping is better for reducing sleep apnea than back sleeping. Research shows that in many cases, sleeping on your side can significantly reduce breathing disruptions from both OSA and CSA. However, the reasons for symptom improvement differ between the two types of sleep apnea.
When sleeping on your side, it is less likely that tissues in your mouth and throat will move into a position where they can block your airway. For this reason, many doctors recommend side sleeping as part of a plan to address OSA. Sleeping on your side can also reduce snoring , which is a common symptom of sleep apnea.
One study found that sleeping on your right side is the best position for reducing OSA , likely due to differences in blood flow to and from the heart. However, left-side sleeping may be more appropriate under certain circumstances. For example, if you have gastroesophageal reflux disease (GERD) at night, you may find more symptom relief by sleeping on your left side . Experts also recommend sleeping on your left side if you are pregnant because this position may reduce pressure on the liver and promote healthy blood flow.
CSA is not caused by a blocked airway, yet research shows that side sleeping can reduce breathing problems tied to the condition. Experts hypothesize that sleeping position may affect breathing in CSA by altering both the amount of space available in the lungs and the relay of signals between the brain and body that control your rate of breathing. However, it is important to note that the positive effects of side sleeping are generally greater for OSA than CSA.
How to Sleep on Your Side
Most adults prefer to sleep on their side, but if this is not your natural sleeping position, you can try different approaches to changing your sleep posture.
One way to stay on your side is to use pillows in one or more places on your bed that help keep from rolling onto your back. You can experiment with different sizes of pillows and where to align them.
Another method to help sleep on your side is to put a tennis ball inside a sock and sew the sock to the back of a shirt. If you roll onto your back, the ball may cause enough discomfort to cause you to change positions without waking you up.
In some cases, health care providers may recommend positioning devices that vibrate if you start to sleep on your back. However, research on the effectiveness of these devices is limited.
A mattress and pillow that appropriately support your body can help promote comfort when sleeping on your side. You might also benefit from sleeping with a pillow between your knees or a body pillow for additional support.
Sleeping on Your Stomach
Research on stomach sleeping and OSA and CSA symptoms is limited, and evidence from the few available studies is mixed.
Results from some small studies suggest that stomach sleeping can reduce pauses in breathing from obstructive sleep apnea. As with side sleeping, sleeping on your stomach may prevent the airway from being blocked. However, given the lack of extensive studies, the evidence about the impacts of stomach sleeping on OSA is far from conclusive.
Sleeping on your stomach is the least popular sleep position among adults. In this position, you may experience difficulty sleeping. In some cases, stomach sleeping leads to rotation of the neck , back pain, or unwanted awakenings.
Stomach Sleeping and CPAP
Sleeping on your stomach may make it hard to use continuous positive airway pressure (CPAP) devices, which are commonly used to treat sleep apnea. CPAP machines require you to wear a face mask that delivers pressurized air to your nose or mouth, and stomach sleeping may not be compatible with the mask.
Being on your stomach may press the mask into your face and cause discomfort. The mask may also shift out of place and leak air , which can cause dry eyes and reduce the effectiveness of PAP therapy.

Sleeping on Your Back
Experts advise that you should try to avoid sleeping on your back if you have OSA. In this position, gravity can cause the tongue to fall back in the mouth where it can obstruct the flow of air through the throat. As a result of its narrowing effect on the airway, back sleeping can also worsen snoring .
Although CSA is caused by the brain’s failure to regulate breathing rather than a blocked airway, research shows that CSA-related breathing problems occur more frequently when you are on your back . As a result, back sleeping may worsen symptoms of CSA.
If you have OSA or CSA and prefer to sleep on your back, you may find a compromise by sleeping with your head up at a 60-degree angle. Sleeping in an elevated position can limit how much gravity pulls the tongue and other tissues into a position where they can block the airway. Sleeping with your head elevated can also reduce snoring.
Best Head Position for Sleep Apnea
Because OSA is caused by a blocked airway, the best head position for sleep apnea is one that keeps the airway open. The optimal way to rest your head may depend on your overall sleeping position, but, in general, it may be best to avoid being face up while in bed.
If you sleep on your side, you may naturally face toward the side when you sleep. If you tend to sleep on your back, one small study found that you may be able to reduce breathing disruptions from sleep apnea if you turn your head to the side while in this position.
In any sleep position, your head should be positioned in line with your neck and spine. When on your side, you may require a taller pillow to avoid neck strain and to ensure that your spine stays aligned. A rolled towel near your pillow may also provide extra height and support for your neck.
If you sleep on your back, you may consider a pillow or other accessory that keeps your head and upper torso at an elevated angle while you sleep. If you sleep on your stomach, you generally do not require much pillow height or neck support.
Take Our Quiz to Know Your Sleep Apnea Risk
To understand if you could have sleep apnea, take our short quiz below to see if you exhibit any signs.
Managing Sleep Apnea Symptoms for Better Sleep
Experts typically recommend that people with sleep apnea avoid back sleeping, but they also generally suggest other treatments as well. The most appropriate sleep apnea treatment depends on the type of sleep apnea, its severity, and other aspects of a person’s overall health. There are a number of treatment options available for sleep apnea.
- Continuous positive airway pressure (CPAP): A CPAP machine pumps air into a face mask at a consistent level of pressure. This pressurized air helps hold the airway open. Both people with OSA and people with CSA may benefit from CPAP therapy.
- Other types of PAP therapy: In some cases, sleep apnea treatment uses another type of positive airway pressure (PAP), such as auto-adjusting PAP (APAP) or bilevel PAP (BiPAP). Like a CPAP, these devices pump pressurized air into the airway, but they use different methods for setting and controlling the amount of air pressure.
- Oral appliances: For people with OSA, oral appliances help keep the airway open by repositioning the jaw or tongue. Oral appliances are often the next choice of treatment if CPAP therapy is not comfortable or effective.
- Surgery: Different surgical options are available for some cases of OSA and CSA. Surgery types vary depending on the cause of sleep apnea but include tonsil or adenoid removal, modification of the anatomy of the nose or throat, and phrenic or hypoglossal nerve stimulation.
- Treating underlying causes: Some conditions, such as heart failure or chronic opioid use, can trigger or worsen CSA. By treating these conditions, people may see their CSA symptoms lessen or resolve.
In addition to these treatment approaches, doctors may suggest lifestyle changes that can help address sleep apnea.
- Avoiding alcohol: Experts recommend that people with OSA or people who snore avoid drinking alcohol before they go to sleep because alcohol can slow down the nervous system and make tissue more likely to block the airway.
- Evaluating medications. Certain medications can affect OSA or CSA symptoms. A reduction in the use of these drugs or avoidance of them altogether may improve sleep apnea symptoms. Be sure to consult a health care provider before changing or ceasing the use of a medication.
The optimal treatment and lifestyle changes for sleep apnea can vary based on the individual. For that reason, it is important to discuss treatment options with a doctor who can describe the potential benefits and downsides of each approach and suggest a tailored treatment plan.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
10 Sources
-
Pinna, G. D., Robbi, E., La Rovere, M. T., Taurino, A. E., Bruschi, C., Guazzotti, G., & Maestri, R. (2015). Differential impact of body position on the severity of disordered breathing in heart failure patients with obstructive vs. central sleep apnoea. European Journal of Heart Failure, 17(12), 1302–1309.
https://pubmed.ncbi.nlm.nih.gov/26467056/ -
Strohl, K. P. (2022, October). Sleep apnea. Merck Manual Consumer Version., Retrieved January 5, 2023, from
https://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea -
Ozeke, O., Erturk, O., Gungor, M., Hızel, S. B., Aydın, D., Celenk, M. K., Dıncer, H., Ilıcın, G., Ozgen, F., & Ozer, C. (2012). Influence of the right- versus left-sided sleeping position on the apnea-hypopnea index in patients with sleep apnea. Sleep and Breathing, 16(3), 617–620.
https://pubmed.ncbi.nlm.nih.gov/21678115/ -
Khoury, R. M., Camacho-Lobato, L., Katz, P. O., Mohiuddin, M. A., & Castell, D. O. (1999). Influence of spontaneous sleep positions on nighttime recumbent reflux in patients with gastroesophageal reflux disease. The American journal of gastroenterology, 94(8), 2069–2073.
https://pubmed.ncbi.nlm.nih.gov/10445529/ -
Bidarian-Moniri, A., Nilsson, M., Rasmusson, L., Attia, J., & Ejnell, H. (2015). The effect of the prone sleeping position on obstructive sleep apnoea. Acta Oto-Laryngologica, 135(1), 79–84.
https://pubmed.ncbi.nlm.nih.gov/25384381/ -
Menon, A., & Kumar, M. (2013). Influence of body position on severity of obstructive sleep apnea: A systematic review. ISRN Otolaryngology, 2013, 670381.
https://pubmed.ncbi.nlm.nih.gov/24223313/ -
Lebret, M., Arnol, N., Martinot, J. B., Lambert, L., Tamisier, R., Pepin, J. L., & Borel, J. C. (2018). Determinants of unintentional leaks during CPAP treatment in OSA. Chest, 153(4), 834–842.
https://pubmed.ncbi.nlm.nih.gov/28847549/ -
Ravesloot, M. J., van Maanen, J. P., Dun, L., & de Vries, N. (2013). The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea: A review of the literature. Sleep and Breathing, 17(1), 39–49.
https://pubmed.ncbi.nlm.nih.gov/22441662/ -
Badr, M. S. (2021, April 15). Central sleep apnea: Pathogenesis. In R. D. Chervin (Ed.). UpToDate., Retrieved January 5, 2023, from
https://www.uptodate.com/contents/central-sleep-apnea-pathogenesis -
Zhu, K., Bradley, T. D., Patel, M., & Alshaer, H. (2017). Influence of head position on obstructive sleep apnea severity. Sleep and Breathing, 21(4), 821–828.
https://pubmed.ncbi.nlm.nih.gov/28608295/










