When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
CPAP Titration Sleep Study
People with sleep-related breathing disorders, like obstructive sleep apnea (OSA) or central sleep apnea (CSA), experience lapses in breathing as they sleep. These breathing issues can cause brief awakenings throughout the night, increasing the likelihood of side effects such as excessive daytime sleepiness, fatigue, or trouble staying asleep.
Continuous positive airway pressure treatment, referred to as CPAP therapy, is a sleep apnea treatment that uses a CPAP machine to blow air into a person’s nose or mouth to keep their airway open . A CPAP titration sleep study is sometimes used to determine the rate at which air should be pushed out of the CPAP machine.
Suspect You May Have Sleep Apnea?
Answer three questions to understand if you should be concerned.
What Is a CPAP Titration Sleep Study?
A CPAP titration sleep study is used to determine the ideal rate of airflow needed to treat a person with a sleep-disordered breathing disorder. This type of sleep study involves connecting a person to a CPAP machine while they spend the night in a sleep laboratory. While using a CPAP machine, the sleeper undergoes polysomnography, which is a standard overnight sleep study that measures various physical markers .
CPAP titration sleep studies generally follow specific steps to calibrate the appropriate rate of airflow to support breathing.
- The CPAP machine is connected to the sleeper and turned on at a low air pressure rate.
- As the person sleeps, the rate of airflow is increased in small increments.
- When a rate successfully opens the person’s airway so they no longer have lapses in breathing, that number is chosen as the fixed rate for the sleeper’s CPAP machine.
- If a person continues to have trouble sleeping while connected to the CPAP machine, humidity might be added to the CPAP air.
- If a sleeper is still experiencing lapses in breathing at a high rate of air flow or is having trouble tolerating the CPAP therapy, they may be put on a bilevel positive airway pressure (BiPAP) machine. BiPAP is another type of sleep apnea treatment.
A CPAP titration sleep study is generally only needed for people who are being prescribed a CPAP machine that emits air at a fixed rate all night. Auto-titrating CPAP machines (APAPs) continually adjust based on the sleeper’s needs throughout the night and do not need to be calibrated by professionals.
Full-Night vs. Split-Night CPAP Titration Study
A full-night CPAP titration study is prescribed for people who have already been diagnosed with a sleep-related breathing disorder. The sole purpose of a full-night study is to calibrate the CPAP machine’s airflow rate to the sleeper’s needs.
In a split-night study, the first portion of the night is used to diagnose the cause of sleep-related breathing issues. If a sleep-related breathing disorder is diagnosed, the remaining time is used to titrate a CPAP machine. If there is not enough time to properly calibrate the CPAP machine to the sleeper’s needs, a follow-up full-night titration study might be ordered.
When a person suspected of having a sleep-related breathing disorder undergoes a diagnostic sleep study, they do not know in advance if it will become a split-night study . A sleep study may become a split-night study if the sleeper is found to have symptoms of moderate to severe obstructive sleep apnea for at least two hours and at least three hours are remaining for CPAP titration.
What to Expect During a CPAP Titration Sleep Study
A sleep study generally involves connecting the sleeper’s body to a variety of monitoring tools, such as those that measure heart activity, breathing, blood oxygen levels, snoring volume, and body position. During a sleep study, a technologist watches and listens to the sleeper from another room, using an infrared camera and microphones connected to the sleeping space.
To conduct CPAP titration, the technologist connects the sleeper to a nearby CPAP machine using a tube and mask. In a full-night study, the sleeper is connected to the CPAP for the entire study. In a split-night study, they are connected for at least three hours of the study.
There are multiple CPAP mask types available, and the technologist might swap out masks throughout the night to see which type works best. They then take notes regarding how well a mask fits and if it leaks air.
Sleep studies rarely have complications, but some people feel uncomfortable sleeping in the lab. The various monitors attached to the body can also cause some people discomfort or skin irritation.

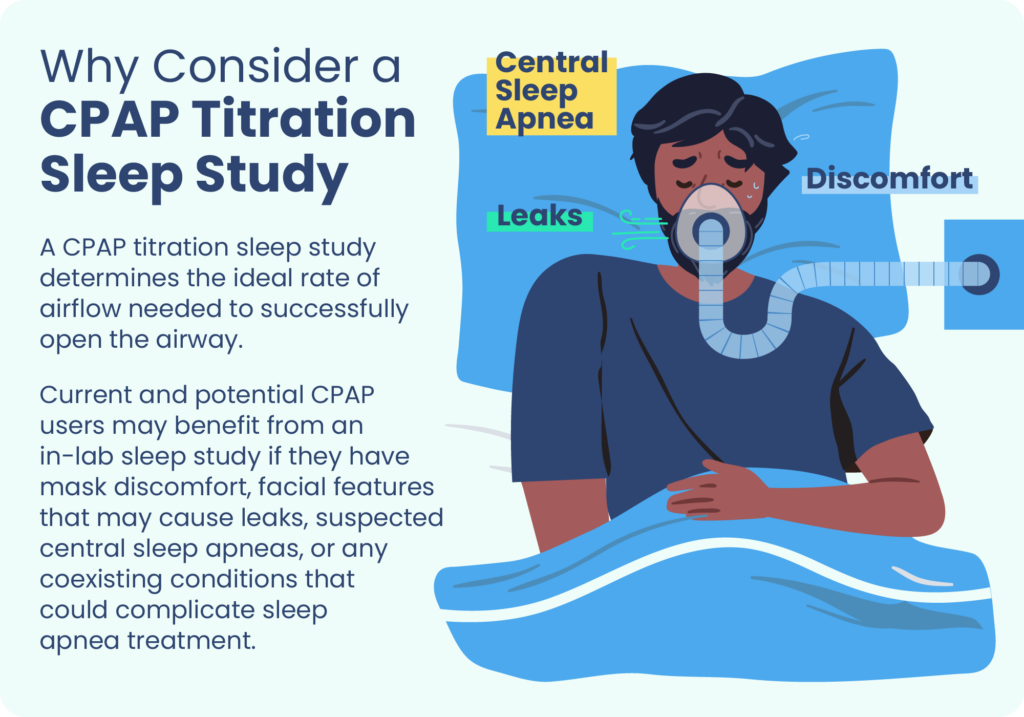
Who a CPAP Titration Sleep Study Is Best For
A CPAP titration sleep study is given to some, but not all, people who have been diagnosed with a sleep-related breathing disorder. At-home CPAP titration is another option, using an auto-CPAP or APAP machine. Experts usually opt for an in-lab CPAP titration sleep study for sleepers with certain characteristics :
- Obstructive sleep apnea that is complicated due to certain coexisting conditions such as pulmonary disease or congestive heart failure
- Facial features that may cause a CPAP mask to leak
- Suspected central sleep apneas, or lapses in breathing caused by the brain
- The need to test out a variety of CPAP mask types
- Previously unsuccessful at-home titration using APAP
- The presence of mental or physical health issues that might interfere with at-home CPAP titration
- Situations that make at-home titration difficult, like people experiencing homelessness or living in a nursing home
When You Should Consider Doing a CPAP Titration Sleep Study
If you have been diagnosed with obstructive sleep apnea or another form of sleep-disordered breathing, your sleep specialist might prescribe you a CPAP titration sleep study.
If you are already using a CPAP machine to treat a sleep-related breathing disorder and suspect that the airflow pressure is too high or too low, you could also ask your sleep specialist about undergoing CPAP titration.
How to Prepare for a CPAP Titration Sleep Study
Before a CPAP titration sleep study, sleepers are often asked to take certain steps to prepare for a sleep study. Preparation may involve:
- Avoiding alcohol and caffeine for a recommended time period prior to the study
- Taking regular medications as usual, unless instructed otherwise
- Taking any additional medications prescribed by the doctor
- Bringing comfortable, loose pajamas and a change of clothes for the next morning
- Arriving with clean hair and skin, free from products or lotion
- Bringing a pillow if desired
- Asking to view the sleep lab in advance if anxiety is an issue
Because each person’s case is unique, it’s important to talk to a doctor or sleep specialist about how to best prepare for a CPAP titration sleep study. Do not change or stop taking any medications without first consulting a doctor.
Receiving Your CPAP Titration Sleep Study Results
By the end of your CPAP titration sleep study, it should be clear what air pressure setting is optimal for your CPAP machine.
If you continue to have symptoms at a high rate of air flow, your sleep specialist may recommend you use a BiPAP machine for treatment instead of a CPAP machine. A BiPAP machine pushes air into the airway, similar to a CPAP, but uses different air pressures for inhalation and exhalation.
CPAP titration results are given one of four ratings:
- Optimal
- Good
- Adequate
- Inadequate
If your results are given an optimal, good, or adequate rating, your sleep specialist might have you use the fixed CPAP air pressure determined during the study. In some cases, good or adequate results are followed up with an at-home titration using an APAP. If your results are determined to be inadequate, an additional CPAP titration sleep study may be required.
Additional Tips for Treating Sleep Apnea
Although CPAP therapy is the primary mode of treatment for obstructive sleep apnea (OSA), there are other actions people can take to reduce the severity of their symptoms.
- Losing weight: Experts generally recommend weight loss for those who have OSA and are obese or overweight, as there is a relationship between weight and sleep apnea. Losing excess weight can reduce the number of times a person with OSA stops breathing during sleep each night.
- Exercising: Engaging in exercise regularly may reduce OSA symptoms.
- Changing sleep positions: Some people experience more severe OSA symptoms when sleeping on their back. In these cases, sleeping on their side may help.
- Avoiding alcohol: Alcohol can make OSA more severe and lead to weight gain. People with untreated OSA should avoid drinking alcohol altogether, not only in the hours before sleeping.
- Checking medications: Some medications can make OSA symptoms worse. Check with a doctor or pharmacist about your current medications to help address any potential side effects.
Talking to Your Doctor About Sleep Apnea and CPAP Therapy
Talk with your doctor if you or someone you share a bed with notice that you are experiencing symptoms associated with sleep-disordered breathing, such as:
- Daytime tiredness
- Snoring during sleep
- Choking or gasping for air during sleep
- Headaches in the morning
- Nighttime awakenings
Obstructive sleep apnea is more common in people with obesity, a large neck, a large waist, or certain medical conditions like high blood pressure and heart failure. Doctors may order a sleep study if some of these risk factors are present, even if the person isn’t aware of symptoms of a sleep-related breathing disorder.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
6 Sources
-
American Academy of Sleep Medicine. (2014). The International Classification of Sleep Disorders – Third Edition (ICSD-3). Darien, IL.
https://aasm.org/ -
Kryger, M. H., & Malhotra, A. (2022, May 23). Management of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate., Retrieved May 19, 2022, from
https://www.uptodate.com/contents/management-of-obstructive-sleep-apnea-in-adults -
Brown, L. K. & Lee, W. (2021, September 17). Titration of positive airway pressure therapy for adults with obstructive sleep apnea. In N. Collop (Ed.). UpToDate., Retrieved May 19, 2022, from
https://www.uptodate.com/contents/titration-of-positive-airway-pressure-therapy-for-adults-with-obstructive-sleep-apnea -
Kramer, N. R. & Millman, R. P. (2021, November 5). Overview of polysomnography in adults. In S. M. Harding (Ed.). UpToDate., Retrieved May 19, 2022, from
https://www.uptodate.com/contents/overview-of-polysomnography-in-adults -
Kline, L. R. (2022, April 1). Clinical presentation and diagnosis of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate., Retrieved May 19, 2022, from
https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults -
Freedman, N. & Kuzniar, T. J. (2021, March 4). Mode selection for titration of positive airway pressure in adults with obstructive sleep apnea. In S. M. Harding (Ed.). UpToDate., Retrieved May 19, 2022, from
https://www.uptodate.com/contents/mode-selection-for-titration-of-positive-airway-pressure-in-adults-with-obstructive-sleep-apnea