Why Can't Hawaii Sleep? And What Makes the Top States For Sleep So Good?
Hawaii conjures many images: pristine beaches, stunning volcanoes, and tourists soaking in the sights.
Add restless nights to the list?
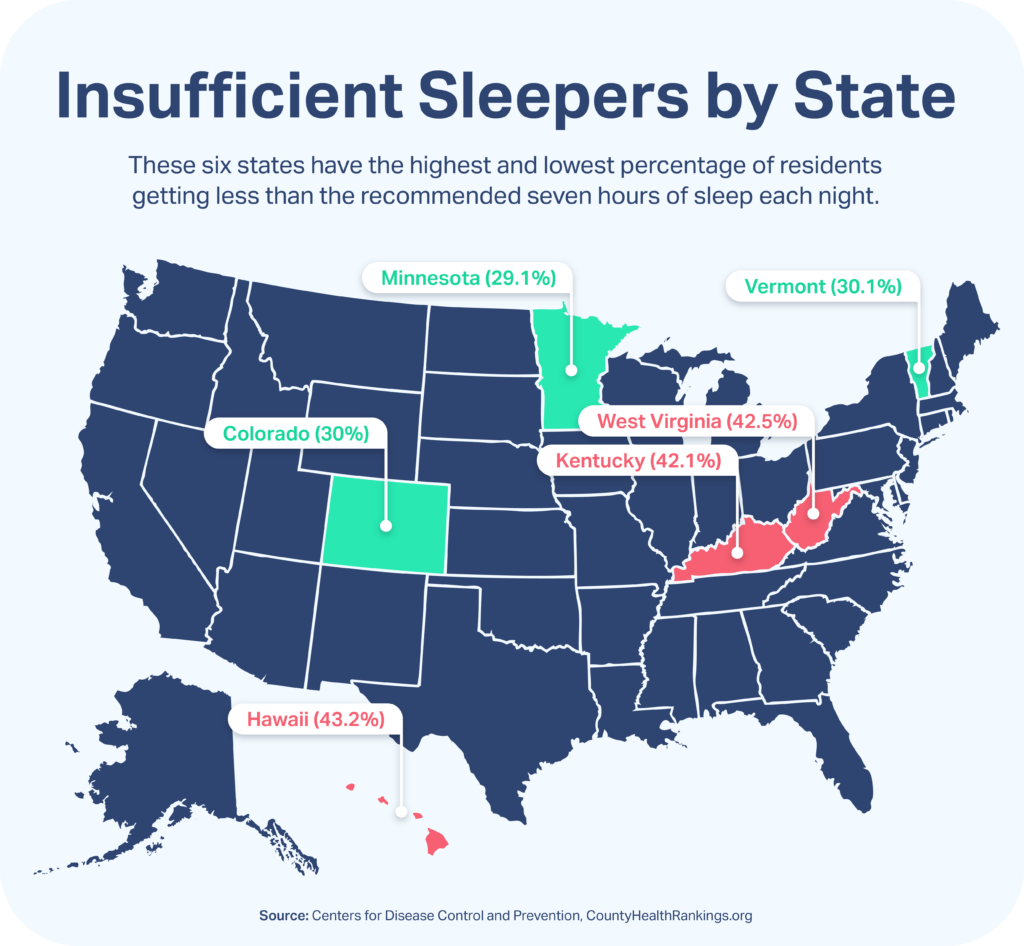
Among all states, Hawaii has the highest percentage of adult residents getting insufficient sleep, according to the 2022 County Health Rankings & Roadmaps report . “Insufficient sleep” is defined as sleeping less than the seven hours each night that the American Academy of Sleep Medicine , Sleep Research Society, and others recommend.
Surprising? Well, it’s not a first. Hawaii had the same dubious honor in 2016, based on 2014 data from the Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System , a state-based telephone survey.
Not getting enough consistent sleep is considered a public health concern. It can lead to chronic conditions and potential workplace hazards. Insufficient sleep also contributes to a variety of health issues, including heart disease, high blood pressure, diabetes, kidney disease, and cancer. It can also worsen existing mental health conditions, such as anxiety and depression.
That’s why insufficient sleep, along with several other factors, made the health report. Getting enough sleep is consistently challenging for Americans. According to the County Health Rankings & Roadmaps report, 35.2% of U.S. adults aren’t getting their seven hours.
Why Are Some States Sleeping Better Than Others?
SleepFoundation.org combed through the CDC and county-ranking data, as well as additional sources, to find clues about why some states have higher percentages of insufficient sleepers than others.
After Hawaii (43.2%), West Virginia (42.5%), and Kentucky (42.1%) had the next-highest percentages of insufficient sleep. Minnesota (29.1%), Colorado (30%), and Vermont (30%) had the lowest, hinting at healthier sleep among adult residents of those states.
Some factors stood out. West Virginia and Kentucky have adult obesity rates well above the U.S. average of 32.1% , for instance. Meanwhile, Minnesota, Colorado, and Vermont have obesity rates below the average, as does Hawaii.
Adults with higher body-mass index (BMI) can have a significantly greater chance of having sleep apnea, says Dr. Kevin Postol, Missouri diplomat for the American Academy of Dental Sleep Medicine. Obesity rates can be good indicators of sleep apnea, a sleep-disrupting condition that Dr. Postol says is still widely undiagnosed and often not treated properly.
As for Hawaii, stress may be a culprit. When SleepFoundation.org polled 519 Hawaii residents ages 18 and older on the online-survey platform Pollfish between June 22 and July 29, 2022, 45.1% of respondents said mental health, stress, and anxiety kept them from getting enough sleep. That was the top thing preventing sleep, respondents said, followed by work schedules (29.7%) and sleep environments (24.7%).
“Stress is one of the biggest issues you have with poor sleep,” Dr. Postol says.

What helps people in some states sleep more than those in others? Let’s start with a look at the states at the top and bottom of the insufficient-sleep list to see how a number of key indicators rank versus the national average. Data is from the 2022 County Health Rankings & Roadmaps report, unless otherwise noted, and includes the following:
- Median household income
- Unemployment rate
- Percent of population with severe housing problems, defined as experiencing overcrowding, high housing costs, poor kitchen facilities, a lack of plumbing, or any combination of those
- Commutes longer than 30 minutes, among commuters who drive alone
- Percent of population with limited access to healthy foods
- Percent of population within close proximity to a park, recreational facility, or similar venue for exercising
- Percent reporting 14 or more days of physical or mental distress in an average month
- Population of adults whose body-mass index exceeds the definition of obese
- Preventable hospital stays per 100,000 Medicare enrollees
- Life expectancy
Here’s what we found.

Hawaii
Hawaii’s position as the state with the highest percentage of insufficient sleepers may have historical context, based on its ranking in past years. But as recently as 2009, just 24.2% of adults living in Hawaii said they felt they were not getting enough sleep for more than 14 out of the past 30 days. That’s quite a bit lower than the 43.2% saying they get less than seven hours of sleep in the latest data. And it’s also lower than the 53.6% of Hawaii adults reporting they are not getting enough sleep, according to the 2022 SleepFoundation.org survey.
What changed? Increased cost of living and long work commutes pre-pandemic, may be driving factors.
Dr. Valerie Cacho, internal medicine and sleep medicine physician serving Hawaii and California, sees financial stress and anxiety as sleep disruptors in Hawaii.
“Hawaii is a pretty expensive state to live in,” she says, “and there’s only so many freeways on Oahu.”
According to Dr. Cacho, Hawaii residents may lose sleep to early wakeup times — don’t forget that its time zone is three hours behind the West Coast of the U.S. and six behind the East Coast — and commuting to multiple jobs to support households. Among commuters, 40.9% of Hawaii residents travel more than 30 minutes commuting alone, compared to 36.6% for the U.S. Honolulu County, the state’s largest and home to its biggest metro area, also has the state’s highest rate of insufficient sleep at 47.1%, among Hawaii counties.
Long commutes and tricky remote-work arrangements may place workers in a Catch-22. But it could bode as a positive.
“During the pandemic, I saw patients who didn’t have to commute anymore, and they actually added extra sleep,” Dr. Cacho says.
Even when Hawaii residents get to bed, they may not be getting to sleep. According to the 2022 SleepFoundation.org survey, 53.8% of Hawaii residents say they take more than 20 minutes to fall asleep. That’s well above the normal 10 to 20 minutes , indicating above-average sleep latency.
Other metrics are positive, as Hawaii residents on average have access to good food and exercise opportunities and live longer than the U.S. average. Hawaii also has the nation’s fewest preventable hospital stays, on average. It’s just a matter of getting the recommended seven hours of sleep that may be a challenge.

Kauai (38.1% insufficient sleep)

Honolulu (47.1% insufficient sleep)

Median household income: $83,173 (U.S.: $64,994)
Unemployment: 4.3% (U.S.: 3.6%)
Severe housing problems: 26.4% (U.S.: 17.3%)
Long commute: 40.9% (U.S.: 36.6%)

Limited access to healthy foods: 5.4% (U.S.: 6.1%)
Access to exercise opportunities: 90% (U.S.: 79.8%)

Frequent physical distress: 9.8% (U.S.: 11.7%)
Frequent mental distress: 11.5% (U.S.: 14.1%)
Adult obesity: 25.5% (U.S: 32.1%)
Preventable hospital stays per 100,000 Medicare enrollees: 1,841 national 3,770
Life expectancy: 80.9 (U.S.: 78.8)

West Virginia
West Virginia has the second-highest percentage of insufficient sleepers among states, with 42.5% of adults getting less than seven hours of sleep. Known for its mountains and mining, West Virginia’s other notable traits may contribute to this ranking.
“We have the reputation in West Virginia of being the most overweight in the nation,” says Dr. George Luis Leon Zaldivar, internal- and sleep-medicine provider at Charleston Area Medical Center in Charleston, West Virginia.
📝 Got a hot tip? Pitch us your story idea, share your expertise with SleepFoundation.org, or let us know about your sleep experiences right here.
According to the County Health Rankings & Roadmaps report, West Virginia’s adult obesity rate is 39.7%, second-highest behind Mississippi at 41.2% Sleep apnea is considered to be most common among adults who are overweight or obese, and it can have a negative effect on sleep if undiagnosed.
Dr. Zaldivar says sleep apnea is common in his state — although he notes it’s an issue all over the U.S. He believes reports of insufficient sleep could, in part, be a combination of people who haven’t been diagnosed with sleep apnea and people who haven’t been treated effectively. West Virginia had the highest percentage (24.3%) of residents in the country who reported their health as poor or fair, per the County Health Rankings & Roadmaps report.

Jefferson (38.6% insufficient sleep)

Mingo (48.7% insufficient sleep)

Median household income: $48,037 (U.S.: $64,994)
Unemployment: 3.6% (U.S.: 3.6%)
Severe housing problems: 11.1% (U.S.: 17.3%)
Long commute: 33.9% (U.S.: 36.6%)

Limited access to healthy foods: 7.5% (U.S.: 6.1%)
Access to exercise opportunities: 49.9% (U.S.: 79.8%)

Frequent physical distress: 17.4% (U.S.: 11.7%)
Frequent mental distress: 22.3% (U.S.: 14.1%)
Adult obesity: 39.7% (U.S.: 32.1%)
Preventable hospital stays: 5,339 (U.S.: 3,770)
Life expectancy: 74.5 (U.S.: 78.8)

Kentucky
Among states, Kentucky has the third-highest percentage of residents getting less than seven hours of sleep each night, at 42.1% of adults . But it’s also home to perhaps the least-sleeping county in the country: McCreary County, whose 49% of insufficient sleepers is the highest among all U.S. counties.
Sample size may be a factor. Sitting in the Daniel Boone National Forest, McCreary has a population of just 16,891 , as of 2021. With a high poverty rate and more than 50% of residents earning less than $20,000 in recent years, it has regularly appeared on “poorest counties in the country” lists.
Trends in the mining-dependent area carry throughout the state. Like West Virginia, Kentucky’s adult obesity rate is higher than the national average. The percentage of people who report frequent mental distress in Kentucky is 18%, compared with a 14.1% national average. Stress, anxiety, and depression can all be linked to a lack of sleep.
Not getting enough physical activity during the day could negatively impact sleep quality at night, and fewer Kentuckians reported access to exercise opportunities than the national average of 79.8%.

Oldham (38.6% insufficient sleep)

McCreary (49% insufficient sleep)

Median household income: $52.238 (U.S.: $64,994)
Unemployment: 3.7% (U.S.: 3.6%)
Severe housing problems: 13.5% (U.S.: 17.3%)
Long commute: 30.4% (U.S.: 36.6%)

Limited access to healthy foods: 6.4% (U.S.: 6.1%)
Access to exercise opportunities: 65.8% (U.S.: 79.8%)

Frequent physical distress: 15.6% (U.S.: 11.7%)
Frequent mental distress: 18% (U.S.: 14.1%)
Adult obesity: 36.4% (U.S.: 32.1%)
Preventable hospital stays: 4,985 (U.S.: 3,770)
Life expectancy: 75.5 (U.S.: 78.8)

Minnesota
The Land of 10,000 Lakes has the lowest percentage of people getting less than seven hours of sleep, at 29.1% of adults . So what are Minnesotans doing differently?
They’re eating healthy and can exercise, even with those frigid Minnesota winters. Its top two counties, Carver and Wright, are within the Minneapolis-St. Paul metro area. This trait also extends to rural areas, with 1.9% of Minnesota’s population involved in agriculture — more than neighboring Wisconsin, at less than 1%, but well below its neighbors to the West.
“I see a large farming population, and they sleep well,” says Stephanie McGreevy, sleep-medicine nurse practitioner at CentraCare Sleep Center in St. Cloud, Minnesota. “They sleep hard because of that activity.”
She adds that Minnesota primary care providers are doing a better job referring people to see a sleep specialist, when needed. Most of her patients who have been treated for sleep apnea, for instance, have significant changes in their sleep, she says.
Minnesotans average 6.6 hours of sleep, compared to 6.4 for Hawaii residents, according to 2022 SleepFoundation.org polls.
That said, Minnesotans aren’t always feeling great about the sleep they are getting — even if they’re primarily getting the recommended seven hours. According to a SleepFoundation.org survey of 600 Minnesota adults conducted June 22 to 30, 2022, on the online survey platform Pollfish, 50.8% of Minnesotans say that stress and anxiety are keeping them awake. Comparatively, stress and anxiety are preventing sleep for 46.3% of adults in Hawaii, the state with the highest percentage of insufficient sleep, according to a separate SleepFoundation.org survey.

Carver (26.7% insufficient sleep)

Mahnomen (35% insufficient sleep)

Median household income: $73.382 (U.S.: $64,994)
Unemployment: 1.8% (U.S.: 3.6%)
Severe housing problems: 13.1% (U.S.: 17.3%)
Long commute: 31.2% (U.S.: 36.6%)

Limited access to healthy foods: 5.7% (U.S.: 6.1%)
Access to exercise opportunities: 80.7% (U.S.: 79.8%)

Frequent physical distress: 9.3% (U.S.: 11.7%)
Frequent mental distress: 12.1% (U.S.: 14.1%)
Adult obesity: 30% (U.S.: 32.1%)
Preventable hospital stays: 3,138 (U.S.: 3,770)
Life expectancy: 80.4 (U.S.: 78.8)

Colorado
Lower rates of obesity, plus access to exercise and medical care, could explain why Colorado has the second-lowest percentage of insufficient sleepers.
Colorado falls below the national average with 30% of adults reporting getting fewer than seven hours of sleep, on average. The state’s obesity rate is also lower than the national average, coming in at 23.6%.
“We have a good medical infrastructure in most areas of our community,” says Ellen Stothard, research and development director for the Colorado Sleep Institute.
Residents in Eagle and Boulder counties, in the north-central part of the state, report getting more sleep than the national state average. Why? Stothard points to socioeconomic factors such as access to healthy food and recreation opportunities, as well as a younger demographic, particularly in the college town of Boulder, Colorado.

Eagle (26% insufficient sleep)

Pueblo (36.1% insufficient sleep)

Median household income: $75,231 (U.S.: $64,994)
Unemployment: 3.4% (U.S.: 3.6%)
Severe housing problems: 16.1% (U.S.: 17.3%)
Long commute: 36.4% (U.S.: 36.6%)

Limited access to healthy foods: 5% (U.S.: 6.1%)
Access to exercise opportunities: 88.4% (U.S.: 79.8%)

Frequent physical distress: 9.6% (U.S.: 11.7%)
Frequent mental distress: 12.4% (U.S.: 14.1%)
Adult obesity: 23.6% (U.S.: 32.1%)
Preventable hospital stays: 2,160 (U.S.: 3,770)
Life expectancy: 80 (U.S.: 78.8)

Vermont
Among U.S. states, Vermont has the third-lowest percentage of residents getting less than seven hours of sleep, at 30.1% of adults . Like Hawaii, it also may be a story of commuting.
Only 32.2% of Vermonters commute more than 30 minutes while driving alone, lower than the national average of 36.6% and considerably lower than Hawaii’s 40.9%. Population is a factor: Vermont is simply not a large state. Its 645,570 residents clock in just above the least-populated state, Wyoming (581,348). Its largest metropolitan statistical area, Burlington-South Burlington-Barre, is home to 34.1% of those people. And that area’s commute time of 22.8 minutes is not only considerably lower than the 26.9 minutes for the U.S. but also on par with the rest of the state.
Since the pandemic, 83,769 working adults stopped commuting entirely, as well. Burlington, Vermont, also had an above-average share of people walking to work — 6.3% , compared with 2.7% of U.S. residents, according to 2019 data.
Like Colorado and Minnesota, the state’s obesity rate is below the national average. This and other factors may indicate a lower probability of sleep apnea and similar sleep issues.

Washington (28.8% insufficient sleep)

Orleans (36.1% insufficient sleep)

Median household income: $63,477 (U.S.: $64,994)
Unemployment: 2.2% (U.S.: 3.6%)
Severe housing problems: 16.8% (U.S.: 17.3%)
Long commute: 32.2% (U.S.: 36.6%)

Limited access to healthy food: 3% (U.S.: 6.1%)
Access to exercise opportunities: 62.5% (U.S.: 79.8%)

Frequent physical distress: 11.1% (U.S.: 11.7%)
Frequent mental distress: 14.8% (U.S. 14.1%)
Adult obesity: 27.1% (U.S.: 32.1%)
Preventable hospital stays: 2,972 (U.S.: 3,770)
Life expectancy: 79.8 (U.S.: 78.8)
References
20 Sources
-
2022 County Health Rankings National Findings Report. (2022). County Health Rankings & Roadmaps.
https://www.countyhealthrankings.org/reports/2022-county-health-rankings-national-findings-report -
Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S., & Tasali, E. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep, 38(6), 843–844.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4434546/ -
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System CDC – BRFSS. (2022, June 21). Retrieved July 6, 2022, Retrieved July 6, 2022
https://www.cdc.gov/brfss/index.html -
2022 National Statistics Reference Table. County Health Rankings and Roadmap., Retrieved July 6, 2022
https://www.countyhealthrankings.org/sites/default/files/media/document/2022%20National%20Statistics%20Table_0.pdf -
U.S. Census Bureau. (n.d.). MEDIAN INCOME IN THE PAST 12 MONTHS. American Community Survey., Retrieved August 1, 2022, from
https://data.census.gov/cedsci/ -
The Employment Situation. (2022, July 8). [Press release]., Retrieved August 1, 2022, from
https://www.bls.gov/news.release/pdf/empsit.pdf -
Defining Adult Overweight and Obesity. (2022, June 3). Centers for Disease Control and Prevention. Retrieved August 1, 2022, from, Retrieved August 1, 2022, from
https://www.cdc.gov/obesity/basics/adult-defining.html -
(2022). America's Health Rankings | AHR. America's Health Rankings., Retrieved August 1, 2022, from
https://www.americashealthrankings.org -
Life Expectancy at Birth by State. (2019). Centers for Disease Control and Prevention., Retrieved August 1, 2022, from
https://www.cdc.gov/nchs/pressroom/sosmap/life_expectancy/life_expectancy.htm -
Insufficient Sleep Among Hawaii Adults. (n.d.)., Retrieved July 7, 2022
https://www.hawaiihealthmatters.org/content/sites/hawaii/Insufficient_Sleep_Fact_Sheet_2011_HI.pdf -
Jung, D. W., Hwang, S. H., Chung, G. S., Lee, Y. J., Jeong, D. U., & Park, K. S. (2013). Estimation of sleep onset latency based on the blood pressure regulatory reflex mechanism. IEEE journal of biomedical and health informatics, 17(3), 534–544., Retrieved August 1, 2022, from
https://doi.org/10.1109/jbhi.2013.2257816 -
West Virginia Insufficient Sleep. (2022). County Health Rankings. Retrieved July 7, 2022, Retrieved July 7, 2022
https://www.countyhealthrankings.org/app/west-virginia/2022/measure/factors/143/data?sort=sc-2 -
Kentucky Insufficient Sleep. (2022). County Health Rankings. Retrieved July 7, 2022, Retrieved July 7, 2022
https://www.countyhealthrankings.org/app/kentucky/2022/measure/factors/143/data -
U.S. Census Bureau QuickFacts: McCreary County, Kentucky. (2021). Census Bureau QuickFacts. Retrieved August 1, 2022, from, Retrieved August 1, 2022, from
https://www.census.gov/quickfacts/mccrearycountykentucky -
Minnesota Insufficient Sleep. (2022). County Health Rankings. Retrieved July 7, 2022, Retrieved July 7, 2022
https://www.countyhealthrankings.org/app/minnesota/2022/measure/factors/143/data -
Colorado Insufficient Sleep. (2022). County Health Rankings. Retrieved July 7, 2022, Retrieved July 7, 2022
https://www.countyhealthrankings.org/app/colorado/2022/measure/factors/143/data?sort=sc-2 -
Vermont Insufficient Sleep. (2022). County Health Rankings. Retrieved July 7, 2022, Retrieved July 7, 2022
https://www.countyhealthrankings.org/app/vermont/2022/measure/factors/143/data?sort=desc-2 -
U.S. Census Bureau QuickFacts: Vermont. (2022). Census Bureau QuickFacts. Retrieved August 1, 2022, from, Retrieved August 1, 2022, from
https://www.census.gov/quickfacts/VT -
(2022, April 23). 39 million WFH Americans' health has improved since they stopped commuting to work over the pandemic, study reveals. 1AND1 Life. Retrieved August 1, 2022, from, Retrieved August 1, 2022, from
https://www.1and1life.com/blog/wfh-health-commute/ -
U.S. Census Bureau. (2022, July 5). Commuting (Journey to Work). Census.Gov. Retrieved August 1, 2022, from, Retrieved August 1, 2022, from
https://www.census.gov/topics/employment/commuting.html