When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Obstructive Sleep Apnea
What it is, how to recognize it, why it matters, and how it can be treated
- Obstructive sleep apnea (OSA) occurs when the upper airway becomes blocked, leading to brief pauses in breathing during sleep.
- Symptoms include tossing and turning during sleep, snoring, daytime fatigue, and headaches upon waking.
- Treatment options often involve PAP therapy and lifestyle changes to reduce symptoms.
- If you’re concerned your sleep problems are due to sleep apnea, a home sleep test can be a helpful first step in the right direction.
Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated obstruction to the airway during sleep. After a person with OSA falls asleep, their airway intermittently narrows or collapses , causing fragmented sleep and contributing to severe health consequences if left untreated.
Is Your Snoring a Health Risk?
Answer three questions to understand if you should be concerned.
What Is Obstructive Sleep Apnea?
OSA is the most common type of sleep-related breathing disorder, which is a group of sleep disorders marked by abnormal breathing during sleep. There are three other types of sleep-related breathing disorders in addition to obstructive sleep apnea, which differ from OSA in their causes and features.
- Central sleep apnea: Central sleep apnea (CSA) is a disorder in which a person repeatedly stops breathing at night. Unlike OSA, CSA is caused by a lack of signals from the brain that control breathing. Some people have episodes of sleep apnea that have characteristics of both OSA and CSA .
- Sleep-related hypoventilation disorders: With sleep-related hypoventilation, a person’s breathing is inadequate to maintain the appropriate levels of oxygen and carbon dioxide in the blood. While a person can be diagnosed with both OSA and a sleep-related hypoventilation disorder, abnormal levels of oxygen and carbon dioxide typically do not persist as long in people with OSA.
- Sleep-related hypoxemia disorder: A person may be diagnosed with sleep-related hypoxemia disorder if they have low levels of oxygen in their blood that is not caused by another sleep-related breathing disorder like OSA.
Prevalence of Obstructive Sleep Apnea
OSA affects around one billion adults worldwide , though experts believe that actual prevalence may be much higher because the majority of cases go undiagnosed .
Without treatment, interruptions in breathing caused by OSA are associated with significant health consequences . For this reason, it’s important to know the signs of sleep apnea and when to visit a doctor. Learn more about the causes and diagnosis of OSA, as well as treatment options that can restore healthy nighttime breathing.
Symptoms of Obstructive Sleep Apnea
The majority of people with obstructive sleep apnea feel excessively tired during the day and snore loudly at night. However, some people with OSA never develop noticeable symptoms, or they might attribute these signs to another cause. Symptoms of OSA may be present both at nighttime and during the day.
Nighttime symptoms of sleep apnea include:
- Loud snoring
- Tossing and turning during sleep
- Waking up feeling the urge to urinate
- Breathing through the mouth while sleeping
Daytime symptoms of sleep apnea include:
- Waking up feeling tired
- Headaches upon waking
- Dry or sore throat
- Excessive daytime sleepiness
- Trouble with memory or impaired intelligence
- Impotence or decreased sex drive
Signs You May Have Obstructive Sleep Apnea
Symptoms of OSA that occur during sleep can be difficult for a person to detect on their own, and it can take years for an individual to recognize their symptoms and see a doctor. Some of the first noticeable signs of obstructive sleep apnea may include excessive tiredness during the day, reports from loved ones, or early morning symptoms.
- Feeling excessively tired during the day: OSA is the most common medical cause of excessive daytime sleepiness. People with OSA may fall asleep during monotonous activities, like reading or watching TV, and may try to combat persistent sleepiness with caffeine.
- Someone witnesses snoring or apnea: A loved one, caregiver, or bed partner is often the first to notice signs of obstructive sleep apnea . They may report loud, disruptive snoring or hearing a sleeper gasp, choke, snort, or stop breathing during sleep.
- Morning symptoms: Waking up with a headache, dry mouth, or the need to urinate may be signs of underlying OSA. Morning headaches may last for hours and occur most days.
Causes of Obstructive Sleep Apnea
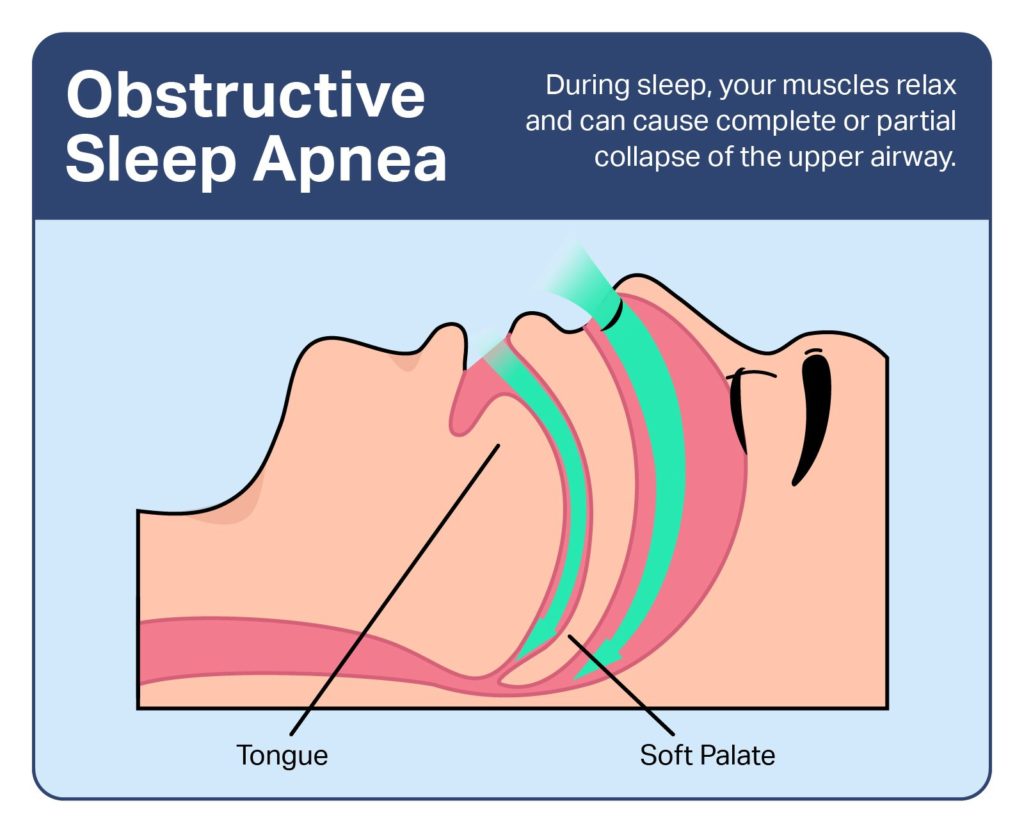
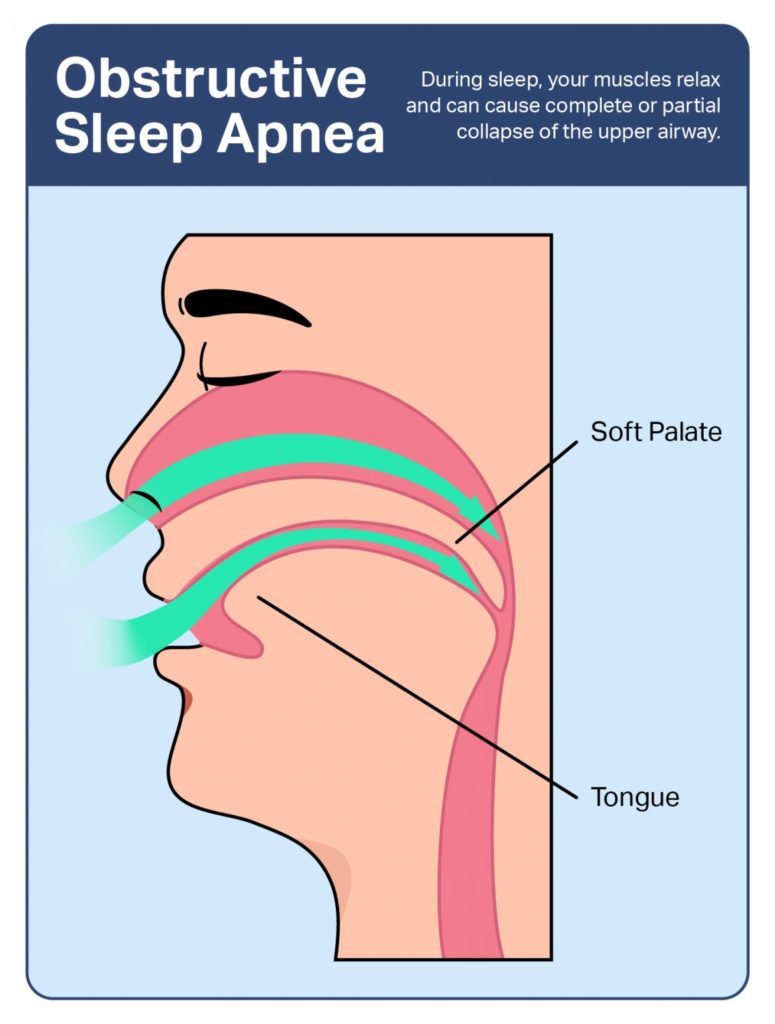
Obstructive sleep apnea typically occurs due to a natural relaxation of the muscles that surround the throat while a person sleeps. During the daytime, these muscles hold the airway open and facilitate breathing. As these muscles relax during sleep, the airway can narrow or close and reduce the space needed for airflow.
For most people, this narrowing of the airway during sleep does not cause any problems. In people who are susceptible to OSA—for example, those with a naturally narrow throat—more severe narrowing causes obstructions and failed attempts to inhale. Trying to inhale against a closed or narrow airway creates abnormal levels of both oxygen and carbon dioxide in the blood, in addition to fragmented sleep.
Airway obstructions may be described as hypopneas or apneas, depending on their severity. When airflow is reduced by at least 30% for 10 seconds or more, the episode may be called a hypopnea. If airflow is reduced 90% or more for at least 10 seconds, it is described as an apnea.
A doctor may diagnose OSA when apneas or hypopneas occur more than five times an hour and are witnessed by a loved one or cause negative health effects.

Risk Factors
Research has identified several factors that increase a person’s risk of developing obstructive sleep apnea.
- Age: The chances of developing OSA increase as a person gets older until around 60 to 70 years old, when the risk levels out.
- Sex: The risk of OSA is highest in men and people assigned male at birth. The risk in women and people assigned female at birth is highest as they become peri- or postmenopausal.
- Body mass index (BMI): The likelihood of developing OSA goes up with a person’s BMI, which is a measure of body fat based on a person’s height and weight.
Certain physical features can also make a person more likely to develop OSA, such as:
- A lower jaw that is small or positioned farther back
- A tongue that is enlarged at its base
- Large tonsils
- A neck size larger than 17 inches
- Excess fat surrounding the throat
There are other risk factors that are still being studied, but may increase a person’s risk of OSA.
- Cigarette smoking: Smoking can increase the risk of OSA by as much as three times compared to people who have quit or who have never smoked.
- Family history: Immediate relatives of people with OSA are twice as likely to develop the condition themselves compared to those in families without OSA. Researchers suggest that this increased risk could be at least partially related to shared anatomical features, similar lifestyles, or a common environment.
- Nasal congestion: A stuffy nose may double a person’s chances of experiencing OSA. Nasal congestion can be caused by a variety of factors, including colds, sinus infections, or the flu.
How is Obstructive Sleep Apnea Diagnosed?
To diagnose obstructive sleep apnea, doctors collect a patient’s medical history and symptoms, conduct a physical exam, and refer them for a diagnostic sleep study.
Medical History
While collecting a person’s medical history, a doctor may inquire about risk factors as well as both nighttime and daytime symptoms. In some cases, a doctor may have a person fill out a questionnaire to look for additional symptoms and help differentiate between OSA and other conditions .
Because sleepers may not recognize their nighttime symptoms, roommates, bed partners, and loved ones may also be asked to report a person’s symptoms.
Physical Exam
Doctors typically perform a physical exam to check for obesity, physical features that increase the risk of OSA, a person’s neck and waist size, and signs of health complications associated with OSA.
Sleep Study
A sleep study can confirm a diagnosis of obstructive sleep apnea and measure the severity of breathing disruptions. Also called polysomnography, a sleep study involves an overnight stay at a specialized sleep laboratory, often located within a sleep center or hospital. Sometimes a sleep study can be completed at home with a portable sleep monitor.
During a sleep study, a trained technician will place sensors on the head and other parts of the body. They may also place several belts around the chest and position a small tube beneath the nose. These devices take measurements of various body functions during sleep, such as breathing, movements, heart rate, and how long it takes to enter different stages of sleep.
A doctor may recommend either a full-night or split-night sleep study.
- Full-night sleep study: A full-night study involves measuring various body functions for the entire night at a sleep laboratory. Because the whole night is used to diagnose OSA, people who are found to have OSA during a full-night sleep study may need a second sleep study for treatment planning.
- Split-night sleep study: A split-night sleep study involves separating the night spent in the sleep laboratory into two portions. The first part of the night is used to diagnose OSA. If the diagnosis is confirmed, the second part of the night is used to plan treatment.
When considered in combination with a person’s symptoms, the number of breathing events per hour found during a sleep study can help doctors determine the severity of OSA.
| Severity of Obstructive Sleep Apnea | Number of Breathing Events per Hour |
|---|---|
| Mild OSA | 5-14 |
| Moderate OSA | 15-30 |
| Severe OSA | More than 30 |
Home Sleep Apnea Testing
While polysomnography conducted in a sleep laboratory is the preferred diagnostic test for obstructive sleep apnea, some people may be eligible for a home sleep apnea test. Home sleep apnea testing may be appropriate for people with a high likelihood of moderate to severe OSA. It may also be required by a person’s health insurance as a preliminary test for OSA.
Individuals undergoing home sleep apnea testing should remain in close contact with their doctor or sleep specialist. A trained medical provider can help ensure that sensors are placed appropriately and will need to interpret the test results.
Treatments
Treatments for obstructive sleep apnea are designed to resolve nighttime breathing disruptions, improve quality of sleep, and reduce health complications. The primary treatment for OSA is positive airway pressure (PAP) therapy.
PAP therapy involves the use of pressurized air, which is pumped through a bedside machine and into the nose and/or mouth to keep the airway open during sleep. PAP therapy may be provided using continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP or BPAP), or auto-titrating positive airway pressure (APAP).
- CPAP: A CPAP machine pumps air at a consistent and predetermined pressure during both inhalation and exhalation, though a release setting may be used to lower the pressure at the beginning of each exhaled breath. CPAP is the type of PAP device used most often in people with OSA.
- BiPAP: BiPAP machines pump air at pre-selected pressures that differ between inhalation and exhalation.
- APAP: APAP differs from other PAP devices in that the air pressure changes in response to signals from the body, including shifts in airflow and snoring. APAP may also be called auto-adjusting CPAP or auto-PAP.
Behavior changes are also an important tool in treating OSA and can help most people better manage their condition.
- Change sleeping position: Some people experience OSA when they sleep on their backs, so avoiding back sleeping may reduce their symptoms. Several methods may help sleepers learn to stop sleeping on their backs, including commercially available straps, training alarms, and attaching a tennis ball to the back.
- Reduce body weight: Weight loss is an important step for people with obesity or OSA that is caused or exacerbated by excess body weight. Exercise alone may also reduce nighttime breathing disruptions, even without weight loss.
- Avoid triggers: Several substances can trigger or worsen OSA and should be minimized or avoided when possible. Alcohol and medications including sedatives can decrease breathing and make it harder to wake up, which can be dangerous in people with OSA.
Other Treatments for Obstructive Sleep Apnea
In people who are unwilling to try, unable to use, or who would not benefit from PAP therapy, doctors may recommend an oral appliance, surgery, or treatment with medications.
- Oral appliances: Oral appliances are removable devices that are worn while sleeping to prevent the airway from closing. Appliances are fitted by a dentist and may shift the lower jaw forward so the tongue cannot block the throat. Oral appliances may be used in people with mild to moderate OSA.
- Surgery: Surgery may be recommended to remove tissue that causes or worsens airway obstructions, such as enlarged tonsils, nasal polyps, and abnormalities of the jaw or tongue. Another type of surgery uses an implanted medical device to stimulate a nerve that controls the tongue.
- Medications: Medications for OSA may be recommended to reduce sleepiness, stimulate breathing, prevent the airway from collapsing during sleep, or treat other causes of OSA. Although many medications have been studied for managing OSA, none have been found to be as effective as PAP therapy and other treatments.
Complications
Untreated obstructive sleep apnea is associated with numerous negative health consequences. Many complications of OSA are caused by a sleeper’s unsuccessful attempts to inhale when their airway is closed or obstructed. These failed inhalations reduce oxygen levels in the blood, increase carbon dioxide, and lead to repeated nighttime awakenings.
Complications of OSA include impared driving, mental health changes, and various medical conditions.
- Drowsy driving: Driving accidents are a significant risk for people with OSA. In fact, people with OSA are two to three times more likely to be in a motor vehicle accident than people without OSA.
- Mental health changes: OSA is associated with a variety of mental health changes, including irritability, depression, and anxiety. People with OSA may also experience impaired attention, memory, and an increased risk of making errors.
- Cardiovascular disease: OSA increases the risk of health conditions affecting the heart and blood vessels, such as hypertension that is difficult to control, an irregular heart beat , and heart failure. OSA also increases the risk of stroke.
- Diabetes: People with OSA have a higher likelihood of insulin resistance, metabolic syndrome, and type 2 diabetes. OSA can also increase the likelihood of developing complications from diabetes.
- Nonalcoholic fatty liver disease: Nonalcoholic fatty liver disease is a condition in which unrelated to alcohol intake. Having OSA increases the chances of developing nonalcoholic fatty liver disease by two to three times.
Living with Sleep Apnea
It’s important for people diagnosed with obstructive sleep apnea to be informed about their diagnosis and the importance of appropriate treatment. While OSA typically cannot be cured, treatment helps most people reduce breathing disruptions, improve sleep quality, and minimize health consequences. The following tips can help people learn to live with OSA.
- Find support: Daily use of PAP therapy or other treatments can be a significant adjustment for people diagnosed with OSA. Connecting with other people with OSA through websites and support groups may be a helpful first step in finding accurate information and social support.
- Be cautious when driving: The side effects of OSA can make it difficult to concentrate and stay alert. People with OSA should be aware of the risks of driving, operating machinery, and performing other dangerous tasks.
- Follow up regularly with a doctor: After a diagnosis of OSA, people should maintain frequent communication with a doctor or sleep specialist. A trained doctor or nurse can help people learn to use their PAP device, address any challenges that arise, ensure that treatment is working, and monitor side effects over time.
- Avoid substances that worsen OSA: For people living with OSA, it’s important to avoid substances that could aggravate breathing issues during sleep. Be sure to talk to a doctor before using sedatives, , benzodiazepines, narcotics, and alcohol.
- Talk to doctors about OSA: To prevent airway obstructions, people with OSA need special care when receiving anesthesia or pain medications, so people should discuss their diagnosis with all doctors and medical professionals.
People living with sleep apnea should also ensure that they get enough sleep each night. In addition to following their prescribed treatment plan, people can improve their sleep by following basic sleep hygiene practices.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
17 Sources
-
Kline, L. R. (2022, June 1). Clinical presentation and diagnosis of obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults -
A.D.A.M. Medical Encyclopedia. (2021, July 12). Central sleep apnea. MedlinePlus.
https://medlineplus.gov/ency/article/003997.htm -
Schulman, D. (2022, January 12). Polysomnography in the evaluation of sleep-disordered breathing in adults. In S. M. Harding (Ed.). UpToDate.
https://www.uptodate.com/contents/polysomnography-in-the-evaluation-of-sleep-disordered-breathing-in-adults -
Theodore, A. C. (2022, June 9). Measures of oxygenation and mechanisms of hypoxemia. In P. E. Parsons (Ed.). UpToDate., Retrieved July 4, 2022, from
https://www.uptodate.com/contents/measures-of-oxygenation-and-mechanisms-of-hypoxemia -
Benjafield, A. V., Ayas, N. T., Eastwood, P. R., Heinzer, R., Ip, M., Morrell, M. J., Nunez, C. M., Patel, S. R., Penzel, T., Pépin, J. L., Peppard, P. E., Sinha, S., Tufik, S., Valentine, K., & Malhotra, A. (2019). Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. The Lancet. Respiratory Medicine, 7(8), 687–698.
https://pubmed.ncbi.nlm.nih.gov/31300334/ -
Auckley, D. (2021, June 24). Sleep disorders in hospitalized adults: Evaluation and management. In R. Benca & N. Collop (Eds.). UpToDate.
https://www.uptodate.com/contents/sleep-disorders-in-hospitalized-adults-evaluation-and-management -
Slowik, J. M. & Collen, J. F. (2022, February 10). Obstructive sleep apnea. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK459252/ -
Memon, J. & Manganaro, S. N. (2021, August 14). Obstructive sleep-disordered breathing. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK441909/ -
A.D.A.M. Medical Encyclopedia. (2020, January 29). Obstructive sleep apnea – adults. MedlinePlus., Retrieved July 4, 2022, from
https://medlineplus.gov/ency/article/000811.htm -
Badr, M. S. (2022, April 15). Pathophysiology of upper airway obstruction in obstructive sleep apnea in adults. In N. Collop (Ed.). UpToDate.
https://www.uptodate.com/contents/pathophysiology-of-upper-airway-obstruction-in-obstructive-sleep-apnea-in-adults -
National Heart, Lung, and Blood Institute. (n.d.). Calculate your body mass index., Retrieved July 4, 2022, from
https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmicalc.htm -
A.D.A.M. Medical Encyclopedia. (2021, July 19). Stuffy or runny nose – adult. MedlinePlus., Retrieved July 4, 2022, from
https://medlineplus.gov/ency/article/003049.htm -
Strohl, K. P. (2020, September). Sleep apnea. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea -
Kim, S. Y. & Naqvi, I. A. (2021, November 14). Neuroanatomy, cranial nerve 12 (hypoglossal). In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK532869/ -
National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. (2012, July 12). Atrial fibrillation. Centers for Disease Control and Prevention.
https://www.cdc.gov/heartdisease/atrial_fibrillation.htm -
A.D.A.M. Medical Encyclopedia. (2021, April 22). Nonalcoholic fatty liver disease. MedlinePlus.
https://medlineplus.gov/ency/article/007657.htm -
National Institute of Neurological Disorders and Stroke. (2022, April 25). Sleep apnea.
https://www.ninds.nih.gov/health-information/disorders/sleep-apnea






















































