Nocturnal Asthma
Asthma is a condition in which a person’s bronchial tubes become swollen. The bronchial tubes are the body’s airways and allow air to move into and out of the lungs. As the airways swell, they lead to symptoms like wheezing, coughing, chest tightness, and shortness of breath. Swollen airways are also more sensitive to allergens and irritants. When asthma symptoms are worse than usual, it’s called an asthma attack, episode, or flare-up.
It’s estimated that asthma affects 1 out of 12 people in the United States, and unfortunately, the prevalence of asthma appears to be increasing. Over the past 40 years, the global prevalence of asthma has increased 50% every decade. While researchers don’t know why this increase is occurring, many researchers speculate that changes in hygiene practices, the use of certain medications in children, increasing rates of obesity, and vitamin D deficiencies may be to blame.
Asthma and Sleep
Whether it’s due to the symptoms of asthma or just staying up too late, missing sleep can make asthma worse. Sleep loss promotes inflammation in the body and affects lung function, increasing the chances of an asthma attack.
A recent study found that people who get fewer than six hours of sleep experience 1.5 times more asthma attacks and have a poorer health-related quality of life than those who sleep the recommended 7 to 9 hours each night. Poor sleep in people with asthma may also be related to the presence of other health conditions, including sleep disorders, and the stimulating effects of asthma medications.
The symptoms of asthma can flare up or get worse at night. Nighttime asthma, called nocturnal asthma, is an experience that can wreak havoc on a person’s sleep and may be a sign of more severe or poorly-controlled asthma.
What is Nocturnal Asthma?
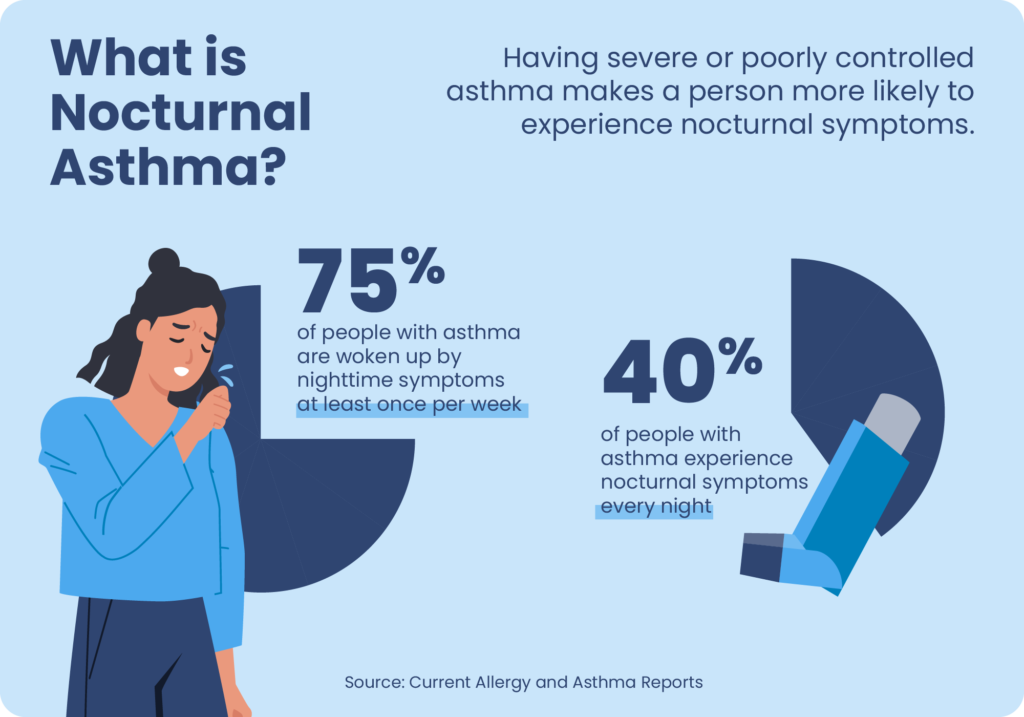
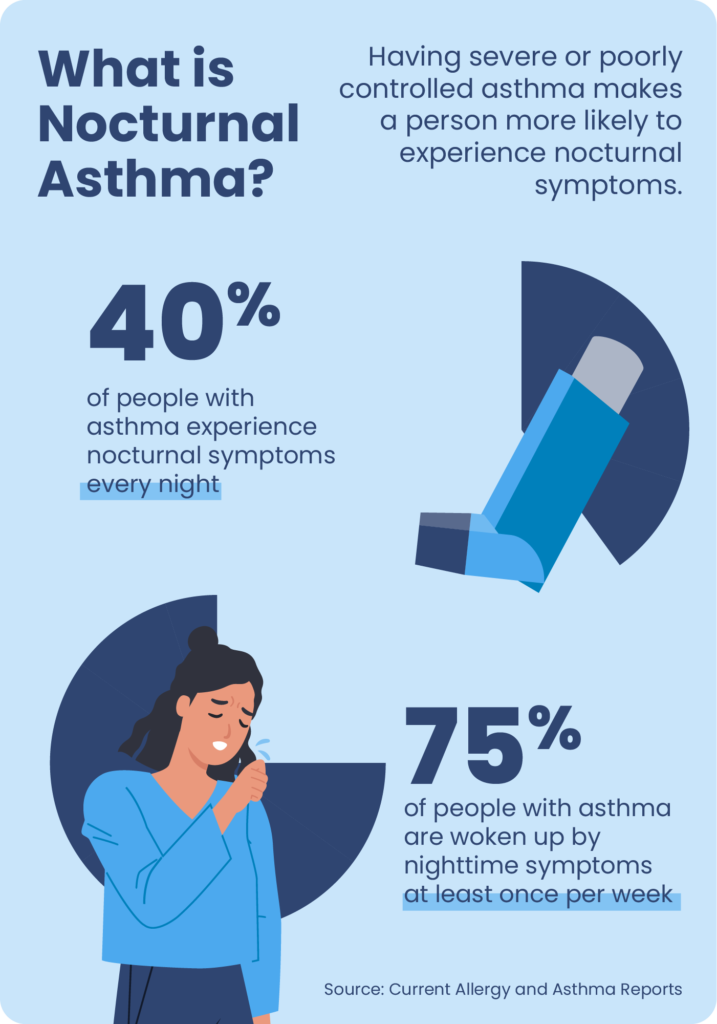
Nocturnal asthma is common, and about 75% of people with asthma are woken up by nighttime symptoms at least once per week. Around 40% of people with asthma experience nocturnal symptoms every night. Having poorly controlled or more severe asthma makes a person more likely to experience nocturnal symptoms.
The mechanisms behind asthma symptoms getting worse at night are not fully understood but may be related to normal hormonal changes in the evening. Many hormones — including epinephrine, cortisol, and melatonin — have circadian patterns, which are 24-hour cycles connected to the body’s internal clock. Changes in these hormones that occur in the evening may contribute to inflammation in the airways, increasing the risk of nocturnal asthma symptoms. Hormonal changes during pregnancy can also affect the symptoms of asthma.
Obesity can also increase the risk of nocturnal asthma and make asthma more difficult to manage. While this link is not fully understood, researchers have hypothesized that excess fat around the throat and increased systemic inflammation may contribute to nocturnal asthma in patients with obesity.
Acid reflux, also called gastroesophageal reflux disease (GERD), is another medical condition commonly associated with nocturnal asthma. As many as 80% of people with asthma also experience GERD symptoms like heartburn and regurgitation.
Nocturnal Asthma Triggers
In addition to obesity, GERD, and circadian hormonal changes, there are many environmental triggers that can provoke nocturnal asthma.
- Tobacco smoke: Smoking and exposure to secondhand tobacco smoke can weaken lung function and irritate the airways.
- Allergens in the bedroom: Many people with asthma are sensitive to dust mites, droppings from pests like cockroaches and rodents, animal dander, mold, and pollen. Even if people are exposed to these allergens during the day, a delayed allergic response can cause asthma to act up after getting into bed.
- Diet: Some people with asthma are sensitive to sulfites in foods and beverages like beer, wine, dried fruit, processed potatoes, and shrimp. If consumed too close to bedtime, these foods may trigger nocturnal asthma.
- Medications: Some medications, including certain cold medicines, aspirin, vitamins, and even eye drops can trigger nocturnal asthma when taken too close to bedtime.
- Cold air: Cold air is a common trigger during the day and can also trigger nighttime symptoms if the bedroom environment is too cold or a window is left open.
- Other medical issues: Viral infections like colds, the flu, and sinus infections are some of the most common triggers for nocturnal asthma attacks.
Nocturnal Asthma and Children
Asthma is more common in children than in adults and is the most common chronic disease in children worldwide. Accurately diagnosing and treating nocturnal asthma in children is especially important because the effects of nocturnal asthma, like loss of sleep and daytime sleepiness, are associated with behavioral and developmental difficulties.
Unfortunately, nocturnal asthma often goes undiagnosed in children because they tend to underestimate or not report their nighttime symptoms. For this reason, it’s helpful for parents to monitor and report back to the doctor any concerning symptoms in children. These symptoms may include wheezing, disturbed sleep, daytime sleepiness, and difficulties concentrating at school.
Asthma and Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a disorder in which the airways narrow or collapse during sleep. Asthma and OSA share similar symptoms and appear to have a bidirectional relationship. This means that having one of these respiratory conditions increases the likelihood of being diagnosed with the other. OSA is particularly common in people with asthma who also snore and those with poorly-controlled asthma symptoms.
People with asthma may find it helpful to talk to their doctors about obstructive sleep apnea. Because asthma puts a person at an increased risk of developing OSA, research suggests that periodic evaluations for OSA may help patients with asthma. Fortunately, treating OSA can often reduce asthma symptoms.
Looking to improve your sleep? Try upgrading your mattress.
Controlling Asthma
Asthma symptoms can often be controlled by working with a doctor, allergist, or pulmonologist (lung specialist) to create a personalized Asthma Action Plan. Controlling asthma typically involves taking asthma medications and making a plan to avoid triggers that make asthma worse. Asthma medications come in two forms: quick-relief medicines that control asthma attacks and long-term control medicines that reduce the frequency and severity of future asthma attacks.
The American Lung Association recommends that people with asthma visit their doctor at least once a year to discuss their Asthma Action Plan. Yet even with the best plan, asthma can sometimes get out of control. If a person with asthma begins to experience new asthma symptoms or starts having trouble with routine activities — like cooking, cleaning, or bathing — it’s important to call a healthcare provider right away.
Avoiding Nighttime Asthma and Improving Sleep
Asthma can make it challenging to get quality sleep, so it’s helpful to cultivate habits that support sleep health. Focusing on improving sleep hygiene is a significant first step. By developing a regular sleep schedule and healthy daytime routines, people with asthma can reduce unnecessary daytime fatigue and focus on controlling their asthma symptoms.
Asthma triggers in the bedroom may increase the risk of nocturnal asthma and lost sleep. In addition to working with a doctor to find solutions for reducing or eliminating asthma triggers, below are a few tips specific to designing the ideal bedroom environment and avoiding nighttime asthma:
- Reducing bedroom allergens: Dust mites and pest residue in the bedroom can trigger nighttime asthma. Eliminating or reducing exposure to these triggers can make a huge difference. Wash bedding regularly and vacuum and dust weekly. Using allergen-proof bedding, like pillows and mattress covers, can help as well. For more information, the Centers for Disease Control and Prevention (CDC) offers a helpful guide to reducing asthma triggers at home.
- Keep pets outside the bedroom: Pet dander and saliva is a common asthma trigger. In addition to regular vacuuming and dusting, it’s helpful to keep pets out of the bedroom in general. For additional protection, consider changing clothes before sleep to prevent tracking pet’s dander into the bedding.
- Be careful with scented products: Strong scents from cleaning products, candles, and personal care products can be a trigger for some people with asthma. Consider making the bedroom an odor- and fragrance-free zone to reduce nighttime asthma.
- De-stress before bed: Stress is a common asthma trigger. Creating a nightly routine that incorporates relaxing activities, like soft music, a warm bath, or reading a book can help people fall asleep faster and reduce stress-related asthma attacks. Our guide to relaxation exercises to help fall asleep may be a helpful resource.
- Close the windows: Many people with asthma know that drastic changes in weather, temperature, and air quality can lead to asthma flare-ups. Reduce temperature changes, pollen, and air pollution in the bedroom by closing bedroom windows. Some people may also benefit from regulating the temperature and humidity in the bedroom environment or getting an air filter.
- Keep asthma medication nearby: Treating nighttime asthma attacks is an important part of controlling asthma. Keep asthma medications, along with a glass of water, near the bed so they are within reach if needed during the night.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
16 Sources
-
Centers for Disease Control and Prevention. (2023, May 10). Asthma in the US., Retrieved January 25, 2021 from
https://www.cdc.gov/asthma/most_recent_national_asthma_data.htm -
Braman S. S. (2006). The global burden of asthma. Chest, 130(1 Suppl), 4S–12S.
https://linkinghub.elsevier.com/retrieve/pii/S0012369215329524 -
American Academy of Allergy, ASthma, and Immunology. (2020, September 28). Increasing rates of allergies and asthma., Retrieved January 25, 2021 from
https://www.aaaai.org/conditions-and-treatments/library/allergy-library/prevalence-of-allergies-and-asthma -
Luyster, F. S., Shi, X., Baniak, L. M., Morris, J. L., & Chasens, E. R. (2020). Associations of sleep duration with patient-reported outcomes and health care use in US adults with asthma. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology, 125(3), 319–324.
https://pubmed.ncbi.nlm.nih.gov/32389780/ -
Irwin, M. R., Wang, M., Campomayor, C. O., Collado-Hidalgo, A., & Cole, S. (2006). Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Archives of internal medicine, 166(16), 1756–1762.
http://archinte.jamanetwork.com/article.aspx?doi=10.1001/archinte.166.16.1756 -
Sutherland E. R. (2005). Nocturnal asthma: underlying mechanisms and treatment. Current allergy and asthma reports, 5(2), 161–167.
https://link.springer.com/10.1007/s11882-005-0091-z -
Calhoun W. J. (2003). Nocturnal asthma. Chest, 123(3 Suppl), 399S–405S.
https://linkinghub.elsevier.com/retrieve/pii/S0012369215352338 -
American Lung Association. (2020, February 27). Asthma and pregnancy.
https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/managing-asthma/asthma-and-pregnancy -
McCallister, J. W., Parsons, J. P., & Mastronarde, J. G. (2011). The relationship between gastroesophageal reflux and asthma: an update. Therapeutic advances in respiratory disease, 5(2), 143–150.
http://journals.sagepub.com/doi/10.1177/1753465810384606 -
A.D.A.M. Medical Encyclopedia. (2020, January 23). Smoking and asthma., Retrieved January 25, 2021, from
https://medlineplus.gov/ency/patientinstructions/000504.htm -
World Health Organization. (2020, May 15). Chronic respiratory diseases: Asthma., Retrieved January 25, 2021 from
https://www.who.int/news-room/q-a-detail/chronic-respiratory-diseases-asthma -
Ginsberg D. (2009). An unidentified monster in the bed–assessing nocturnal asthma in children. McGill journal of medicine, 12(1), 31–38.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2687912/ -
Teodorescu, M., Polomis, D. A., Teodorescu, M. C., Gangnon, R. E., Peterson, A. G., Consens, F. B., Chervin, R. D., & Jarjour, N. N. (2012). Association of obstructive sleep apnea risk or diagnosis with daytime asthma in adults. The Journal of asthma : official journal of the Association for the Care of Asthma, 49(6), 620–628.
https://pubmed.ncbi.nlm.nih.gov/22742082/ -
Teodorescu, M., Barnet, J. H., Hagen, E. W., Palta, M., Young, T. B., & Peppard, P. E. (2015). Association between asthma and risk of developing obstructive sleep apnea. JAMA, 313(2), 156–164.
https://pubmed.ncbi.nlm.nih.gov/25585327/ -
Alkhalil, M., Schulman, E. S., & Getsy, J. (2008). Obstructive sleep apnea syndrome and asthma: the role of continuous positive airway pressure treatment. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology, 101(4), 350–357.
https://linkinghub.elsevier.com/retrieve/pii/S1081120610603092 -
Centers for Disease Control and Prevention. (2020, December 4). Asthma Action Plans., Retrieved January 25, 2021 from
https://www.cdc.gov/asthma/action-plan/documents/asthma-action-plan-508.pdf








