Alzheimer’s Disease and Sleep
Alzheimer’s disease is the most common type of dementia, and symptoms include a progressive, irreversible loss of memory, thinking, reasoning, and other brain functions. As the disease progresses to later stages, affected individuals eventually become unable to care for themselves independently and require caregiver support, either at home or at a long-term care facility.
Alzheimer’s causes sleeping problems that can be disruptive both for the affected patient and for caregivers. People with Alzheimer’s experience sleep disturbances, including shorter or more fragmented sleep, changes to the biological clock and sleep cycle, and certain sleep disorders. Making changes to a patient’s daily schedule and evening habits may improve these sleep issues.
Why Do Alzheimer’s Patients Struggle With Sleep?
Changes in sleep quality and duration in older age are common. However, the sleep concerns seen in people with Alzheimer’s are often more severe and complex. There may be a reciprocal relationship between sleep issues and the other symptoms of Alzheimer’s. This means that sleep loss can worsen other symptoms, such as delusions, restlessness, and wandering, which can, in turn, make sleeping more difficult.
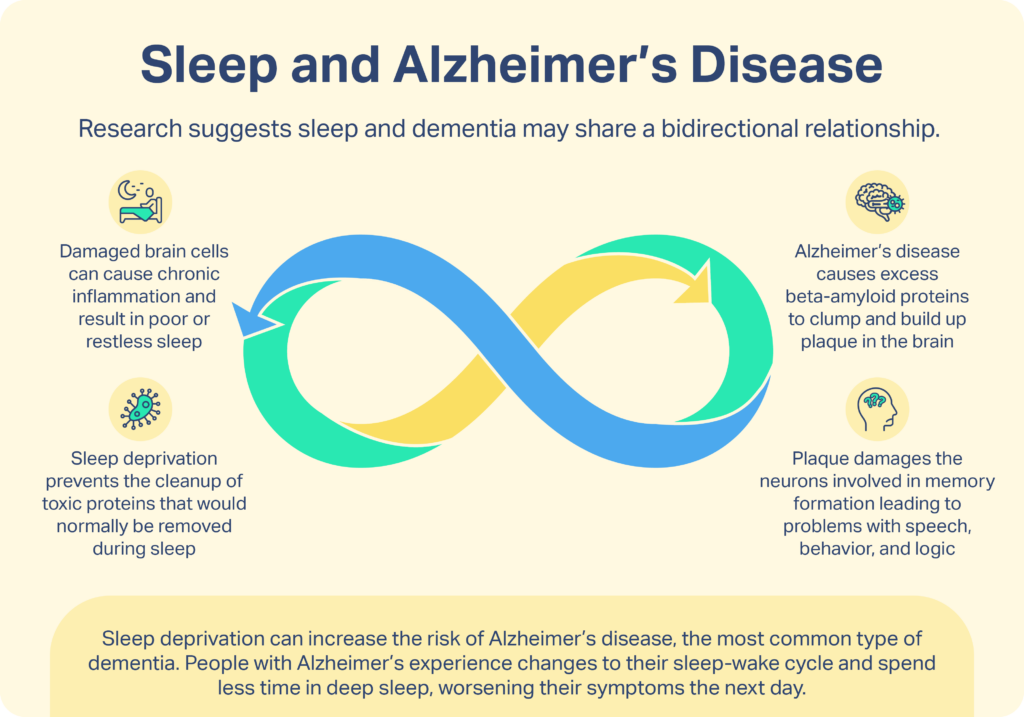
Getting enough sleep and spending sufficient time in deep sleep and rapid eye movement (REM) sleep are necessary in order for preservation of memories to occur. Memory loss is the primary symptom in people living with Alzheimer’s, and compared to older adults without the disease, Alzheimer’s patients spend progressively less time in deep sleep and REM sleep.
People with Alzheimer’s experience dramatic changes to their sleep-wake cycle. The sleep-wake cycle—also called circadian rhythm—is the internal clock in our body that initiates physical processes related to wake and sleep. When this cycle is disturbed in Alzheimer’s patients, the result is not sleeping at night and sleeping too much during the day. Researchers attribute circadian rhythm disruption in Alzheimer’s patients, at least in part, to cellular changes in the brain caused by the disease. Dysregulated production of the sleep hormone, melatonin, in patients with Alzheimer’s may play a role. Other possible factors include decreased physical activity and less natural light exposure.
What Sleep Disorders Are Common in Alzheimer’s Patients?
Having trouble falling and staying asleep, waking up too early, or getting poor quality sleep are hallmark symptoms of insomnia, which is common in people with Alzheimer’s. Other sleep disorders most often seen in this population include the following:
- Obstructive sleep apnea (OSA): OSA is a condition marked by loud snoring, choking, and other respiratory symptoms due to collapse of the airway during sleep. One study found that up to half of Alzheimer’s disease patients develop OSA at some point. Continuous positive airway pressure is the most common treatment for patients with OSA, and it has been found to improve cognition in patients who have both OSA and Alzheimer’s.
- Restless legs syndrome (RLS): In RLS, people experience unsettling crawling or tingling feelings in the legs that they alleviate by moving their legs. The symptoms tend to worsen while resting and can disrupt sleep. A study showed that RLS may be between two and six times more common in cognitively impaired older adults compared to rates seen in healthy older adults. More research is needed to determine whether the widely available RLS treatments are safe and effective for people with Alzheimer’s. However, medical treatment of RLS has shown to improve sleep quality. Medical treatment of RLS improves sleep quality.
- Mood disorders: Many patients with dementia experience depression and anxiety, and these mood disorders are known contributors to sleep problems. Symptoms of depression and anxiety—which can include staying in, withdrawing from social support, and feeling down or upset—can make sleeping more difficult. Cognitive and/or behavioral therapy, sensory stimulation, exercise, and possible use of medications may reduce symptoms of mood disorders and related sleep issues in people with dementia.
Additionally, “sundowning” is a common phenomenon in which people with Alzheimer’s disease experience an increase in symptoms such as confusion, anxiety, and irritability late in the day. It tends to begin around the time the sun sets and can last into the night, affecting sleep. Although the exact cause is unknown, sundowning may be due to disrupted circadian rhythm and/or due to fatigue caused by sleep loss.
How Can Alzheimer’s Patients Get Better Sleep?
Helping an individual with Alzheimer’s to sustain longer, deeper sleep can result in physical health gains and improvement of daytime symptoms that sleep loss causes, such as agitation and disorientation. In addition to treating any underlying sleep disorders that are contributing to disturbed sleep, practicing good sleep hygiene can help people with Alzheimer’s to sleep better. Sleep hygiene means cultivating healthy sleep habits and maintaining an environment that promotes quality sleep. Experiment with the following steps to improve sleep hygiene:
- Balance the daily routine: Incorporate stimulating activities such as errands, family meals, appointments, and exercise into the morning and middle of the day. Reserve evenings for a low-energy routine of soothing activities such as listening to music, reading out loud, and spending time with pets.
- Set a sleep schedule: Going to sleep and waking up at the same time every day can help to regulate circadian rhythm.
- Avoid napping: If possible, napping should be limited because it reinforces dysfunctional sleep-wake patterns and makes it harder to fall and stay asleep at night.
- Add light exposure: Light is the most powerful regulator of circadian rhythm. Spending time outside in natural light may help to reorient the internal clock. Another option is to consider light therapy, which has been shown in some studies to improve sleep symptoms in people with Alzheimer’s. Light therapy involves introducing a specialized, bright lighting device for at least 30 minutes during the day.
- Encourage physical activity: Energy exertion during the day can help with sleeping at night. Walking or doing other exercises outside provide double benefits of both activity and light exposure.
- Manage medication timing: Some medications commonly provided to patients with Alzheimer’s can interfere with sleep if taken late in the day. Talk with a doctor about the ideal time to administer any medications in order to promote healthy sleep.
- Avert hallucinations: If evening hallucinations are delaying or disrupting sleep, it could help to light the room in a way that does not create shadows during the hours leading up to bedtime. Limit bright colors and patterns, avoid loud sounds, and cover mirrors.
These approaches to sleep hygiene may be challenging to implement for some patients, but evidence suggests that such efforts can pay off. A study found that, compared to a control group, implementation of sleep hygiene practices, daily walks, and exposure to a lighting device resulted in a reduction in time awake at night and depression in Alzheimer’s patients and that these gains were sustained after six months.
Is It Safe for Alzheimer’s Patients to Take Sleep Aids? What Should I Do if I Experience Side Effects?
The routine use of medications to treat sleep issues in patients with Alzheimer’s disease is not supported by current scientific evidence. Sleep aids carry extra risks for people with Alzheimer’s; they can cause falls and injury, increase memory loss and confusion, and may have an overly sedative effect. Sleep aids are typically reserved for cases where all other options have been exhausted and should only be given under guidance of a physician.
Melatonin supplements have been studied as a possible option for improving sleep quality in Alzheimer’s patients. However, research examining the effectiveness of melatonin supplements in people with dementia has produced conflicting results. Some studies demonstrated a small benefit, increasing nighttime sleep by around 30 minutes, while other studies showed no benefit. There is also evidence to suggest that melatonin supplements may increase social withdrawal and depression in patients with dementia.
Help for Caregivers
Caring for a person with Alzheimer’s disease requires incredible dedication. Getting quality sleep is critical for patients as well as their caregivers. Caregivers can also benefit from practicing good sleep hygiene habits and tapping into support resources in order to maintain their own health and wellbeing.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
14 Sources
-
National Institute of Neurological Disorders and Stroke. (2022, April, 1). Brain basics: Understanding sleep.
https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep -
Lloret, M. A., Cervera-Ferri, A., Nepomuceno, M., Monllor, P., Esteve, D., & Lloret, A. (2020). Is Sleep Disruption a Cause or Consequence of Alzheimer’s Disease? Reviewing Its Possible Role as a Biomarker. International journal of molecular sciences, 21(3), 1168.
https://pubmed.ncbi.nlm.nih.gov/32050587/ -
Lim, M. M., Gerstner, J. R., & Holtzman, D. M. (2014). The sleep-wake cycle and Alzheimer’s disease: what do we know?. Neurodegenerative disease management, 4(5), 351–362.
https://pubmed.ncbi.nlm.nih.gov/25405649/ -
Mishima, K., Tozawa, T., Satoh, K., Matsumoto, Y., Hishikawa, Y., & Okawa, M. (1999). Melatonin secretion rhythm disorders in patients with senile dementia of Alzheimer’s type with disturbed sleep-waking. Biological psychiatry, 45(4), 417–421.
https://linkinghub.elsevier.com/retrieve/pii/S0006322397005106 -
Emamian, F., Khazaie, H., Tahmasian, M., Leschziner, G. D., Morrell, M. J., Hsiung, G. Y., Rosenzweig, I., & Sepehry, A. A. (2016). The Association Between Obstructive Sleep Apnea and Alzheimer’s Disease: A Meta-Analysis Perspective. Frontiers in aging neuroscience, 8, 78.
https://pubmed.ncbi.nlm.nih.gov/27148046/ -
Rose, K. M., Beck, C., Tsai, P. F., Liem, P. H., Davila, D. G., Kleban, M., Gooneratne, N. S., Kalra, G., & Richards, K. C. (2011). Sleep disturbances and nocturnal agitation behaviors in older adults with dementia. Sleep, 34(6), 779–786.
https://pubmed.ncbi.nlm.nih.gov/21629366/ -
Molano, J., & Vaughn, B. V. (2014). Approach to insomnia in patients with dementia. Neurology. Clinical practice, 4(1), 7–15
https://pubmed.ncbi.nlm.nih.gov/29473586/ -
Burke, A. D., Goldfarb, D., Bollam, P., & Khokher, S. (2019). Diagnosing and Treating Depression in Patients with Alzheimer’s Disease. Neurology and therapy, 8(2), 325–350.
https://pubmed.ncbi.nlm.nih.gov/31435870/ -
National Institute on Aging. (2017, May 17). Tips for Coping with Sundowning., Retrieved November 25, 2020, from
https://www.nia.nih.gov/health/tips-coping-sundowning -
A.D.A.M. Medical Encyclopedia. (2020, April 25). Dementia – behavior and sleep problems.
https://medlineplus.gov/ency/patientinstructions/000029.htm -
National Institute on Aging. (2017, May 17). 6 Tips for Managing Sleep Problems in Alzheimer’s., Retrieved November 25, 2020, from
https://www.nia.nih.gov/health/6-tips-managing-sleep-problems-alzheimers -
Hanford, N., & Figueiro, M. (2013). Light therapy and Alzheimer’s disease and related dementia: past, present, and future. Journal of Alzheimer’s disease : JAD, 33(4), 913–922.
https://pubmed.ncbi.nlm.nih.gov/23099814/ -
McCurry, S. M., Gibbons, L. E., Logsdon, R. G., Vitiello, M. V., & Teri, L. (2005). Nighttime insomnia treatment and education for Alzheimer’s disease: a randomized, controlled trial. Journal of the American Geriatrics Society, 53(5), 793–802.
https://onlinelibrary.wiley.com/doi/10.1111/j.1532-5415.2005.53252.x -
Ooms, S., & Ju, Y. E. (2016). Treatment of Sleep Disorders in Dementia. Current treatment options in neurology, 18(9), 40.
https://pubmed.ncbi.nlm.nih.gov/27476067/

































































