When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
Pregnancy & Sleep: Common Issues & Tips for Sleeping
For many women, sleep can be evasive during pregnancy. Physical discomfort, changing hormones, and excitement and anxiety about being a new mother lead to a host of sleep problems. In fact, it’s believed that at least 50 percent of pregnant women suffer from insomnia.
Sleep is an essential part of prenatal care. If you’re struggling to sleep well during pregnancy, you’re not alone. We’ll discuss common sleep problems for pregnant women, take a look at the best pregnancy sleeping positions, and share advice on how to get the best sleep possible during pregnancy.
Why Does Sleep Change During Pregnancy?
A multitude of factors leads to insomnia during pregnancy. Beginning in the first trimester, fluctuating hormone levels cause generalized discomfort and other problems that can make it difficult to fall asleep and stay asleep. These may include:
- Nausea
- Vomiting
- Breast tenderness
- Increased heart rate
- Shortness of breath
- Higher body temperature
- Frequent nighttime urination
- Leg cramps
As time wears on, expectant mothers may also experience back pain and have trouble finding a comfortable position to accommodate the growing baby bump, especially when the baby starts to kick at night. Anxiety about the upcoming labor, being a new mother, juggling work and home responsibilities, or other worries may keep your mind racing at night. In the third trimester, many pregnant women experience vivid, disturbing dreams that can further impair sleep quality.
While it’s common for most pregnant women to experience at least a few of the above symptoms, sometimes they may be related to a sleep disorder. Sleep disorders can be linked to further problems down the line for mother or baby, so it’s important to talk to your doctor if you’re experiencing any symptoms.
Common Sleep Disorders and Problems During Pregnancy
The most common sleep disorders that tend to occur during pregnancy are obstructive sleep apnea, restless legs syndrome, and gastroesophageal reflux disorder.
- Obstructive Sleep Apnea: Weight gain and nasal congestion lead many women to start snoring during pregnancy, which may be a risk factor for high blood pressure. Some women may go on to develop obstructive sleep apnea (OSA), a sleep condition characterized by snoring, gasping, and repeated lapses in breathing that disrupt sleep quality. OSA may impede oxygen flow to the fetus and increase the risk of preeclampsia, gestational diabetes, and cesarean sections . It is thought to affect as many as 1 in 5 women during pregnancy.
- Restless Legs Syndrome: People with restless legs syndrome (RLS) are plagued by sensations best described as a crawling, tickling, or itching that cause an irrepressible urge to move the legs. This condition can make it difficult to fall asleep, as the symptoms are more severe when the person is at rest. RLS is thought to affect up to one-third of women in their third trimester of pregnancy.
- Gastroesophageal Reflux Disorder: Otherwise known as heartburn or acid reflux, gastroesophageal reflux disorder (GERD) causes an uncomfortable burning sensation in the esophagus, especially when lying down. It’s a common cause of insomnia in pregnant women across all trimesters , thought to affect one-quarter of pregnant women in the first trimester and as many as one-half in the third. Long-term GERD may damage the esophagus.
Help Your Baby Sleep Better With Pediatric Sleep Coaching

our partner at sleepdoctor.com
Learn More“Life-changing! My anxiety about my son’s sleeping habits were immediately reduced after talking to Sara. She went above and beyond to tailor a schedule to our goals, answer our questions, keep us on track, and check in to encourage us when we just thought we couldn’t do it anymore.”
Rachael B. – Verified Customer
Why Is Sleep so Important During Pregnancy?
Getting quality sleep during pregnancy is important for both mother and baby. For the mother, those sleepless nights end up leading to fatigue and daytime sleepiness. Sleep also plays a major role in memory, learning, appetite, mood, and decision-making – all important when preparing to welcome a newborn baby into your home.
Chronic sleep deprivation takes its toll on the immune system. Some researchers believe this may be part of the reason why a lack of sleep has such a significant impact on maternal and fetal health . And since sleep helps regulate blood sugar, it’s not surprising that poor sleep during pregnancy appears to be linked to gestational diabetes mellitus .
Research shows that pregnant women who get too much or not enough sleep in early pregnancy are prone to developing high blood pressure in the third trimester. Severe sleep deprivation in early pregnancy may also raise the risk of preeclampsia , a condition that can lead to preterm delivery and lasting complications for the mother’s heart, kidney, and other organs.
Though more research is needed to control for other variables, poor sleep appears to be a risk factor for preterm birth, low birth weight, painful labor, cesarean delivery, and depression. Emerging evidence also suggests that poor sleep quality during pregnancy may predict sleep problems and crying in babies once they are born.

Treatment for Sleep Problems During Pregnancy
There are a number of ways to reduce sleep problems while pregnant. Principal strategies include adjustments to sleeping position and sleep hygiene habits. In conjunction with good sleep hygiene, managing pregnancy-related sleep disorders is key to getting better sleep while pregnant.
Certain therapies have proven effective for treating sleep disorders, such as a continuous positive airway pressure (CPAP) device for OSA, antacids for GERD, or vitamin and mineral supplements for RLS and other conditions. Although there are many theories, the reason for leg cramps and RLS during pregnancy remains unclear. Suggested therapies include vitamin supplementation, heat therapy, and massage but there is no consensus about what is the best treatment.
As certain substances may pose a risk to the developing fetus, pregnant women should always consult with their doctor before taking any medication or herbal remedies to help with sleep.
Best Sleeping Positions for Pregnancy
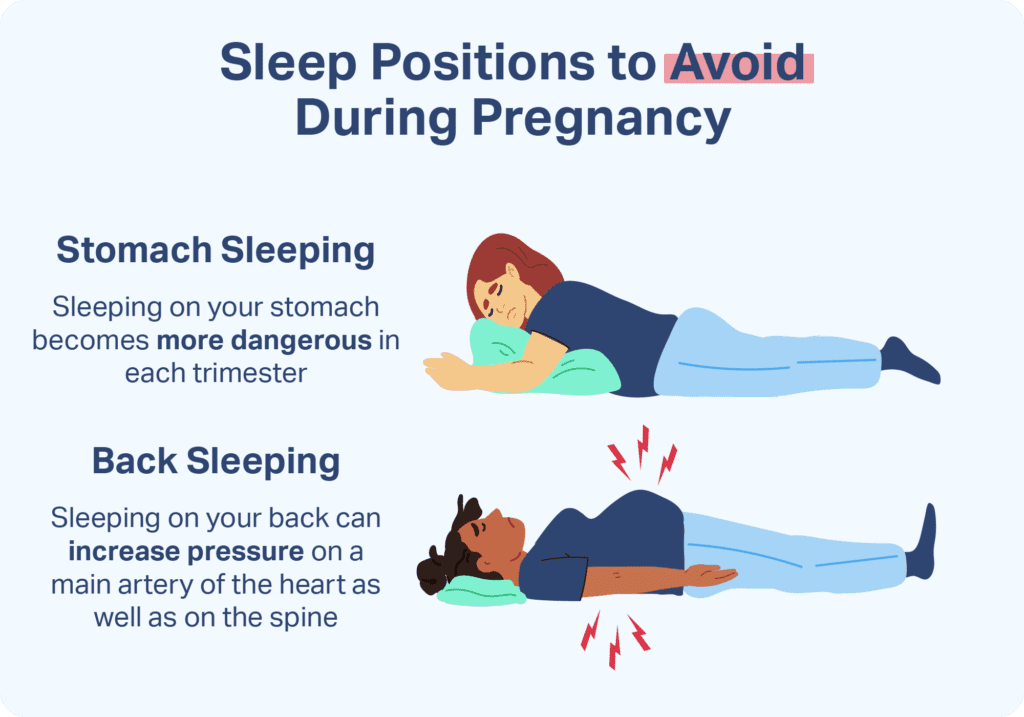
Sleeping on the left side with the legs slightly curled is considered the best sleeping position in pregnancy. This position facilitates blood flow to the heart, kidneys, and uterus, and improves the delivery of oxygen and nutrients to the fetus. Although not as optimal as the left side, sleeping on the right side during pregnancy is also acceptable.

It may be helpful to use a few extra pillows to get comfortable sleeping on your side, especially if you’re not accustomed to this sleeping position. Try tucking in a wedge pillow to support your belly, or adding a thin pillow between the knees to help relieve pressure on the lower back. Some women find it useful to hug a body pillow or place a pillow under the lower back.
As the uterus grows larger, sleeping on the back during pregnancy can cause backache and put pressure on the vena cava. The vena cava is one of the body’s principal veins, so this can interfere with blood flow and cause dizziness. While back sleeping is all right for brief stints, it’s best to avoid it if possible. Most pregnant women find that sleeping on the stomach is impractical once the baby bump reaches a certain size.
Sleep Hygiene for Pregnant Women
Sleep hygiene is more important than ever during pregnancy. In addition to pregnancy sleep aids such as specialized pillows or eye masks, the following habits may help reduce insomnia and improve overall sleep quality:
- Keep a cool, dark, quiet bedroom and limit the bed to sleeping and sex
- Prioritize sleep and stick to a consistent bedtime, scheduling naps earlier in the day so they don’t interfere with nighttime sleep
- Read a book, take a bath, or indulge in another calming activity in preparation for bedtime
- Use a nightlight to make it easier to get back to sleep after bathroom breaks
- Avoid caffeine, spicy foods, and heavy meals too close to bedtime to reduce the risk of GERD
- Avoid taking technology into the bedroom, and turn off screens at least an hour before bed
- Get regular exercise earlier in the day
- Drink plenty of water throughout the day, but reduce liquid intake before bed to reduce nighttime bathroom breaks
- If you can’t sleep, get out of bed and do something else until you feel sleepy
- Write down thoughts in your journal, or seek help from your partner, friends, doctor, or childbirth classes if you’re feeling stressed

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
15 Sources
-
Felder, J. N., Baer, R. J., Rand, L., Jelliffe-Pawlowski, L. L., & Prather, A. A. (2017). Sleep Disorder Diagnosis During Pregnancy and Risk of Preterm Birth. Obstetrics and gynecology, 130(3), 573–581.
https://pubmed.ncbi.nlm.nih.gov/28796676/ -
Won C. H. (2015). Sleeping for Two: The Great Paradox of Sleep in Pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(6), 593–594.
https://pubmed.ncbi.nlm.nih.gov/25979097/ -
Nazik, E., & Eryilmaz, G. (2014). Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women. Journal of clinical nursing, 23(11-12), 1736–1750.
https://onlinelibrary.wiley.com/doi/10.1111/jocn.12323 -
Lara-Carrasco, J., Simard, V., Saint-Onge, K., Lamoureux-Tremblay, V., & Nielsen, T. (2014). Disturbed dreaming during the third trimester of pregnancy. Sleep medicine, 15(6), 694–700.
https://linkinghub.elsevier.com/retrieve/pii/S1389945714001142 -
O’Brien, L. M., Bullough, A. S., Owusu, J. T., Tremblay, K. A., Brincat, C. A., Chames, M. C., Kalbfleisch, J. D., & Chervin, R. D. (2013). Snoring during pregnancy and delivery outcomes: a cohort study. Sleep, 36(11), 1625–1632.
https://academic.oup.com/sleep/article/36/11/1625/2558938 -
Blyton, D. M., Skilton, M. R., Edwards, N., Hennessy, A., Celermajer, D. S., & Sullivan, C. E. (2013). Treatment of sleep disordered breathing reverses low fetal activity levels in preeclampsia. Sleep, 36(1), 15–21.
https://academic.oup.com/sleep/article/36/1/15/2656913 -
Liu, L., Su, G., Wang, S., & Zhu, B. (2019). The prevalence of obstructive sleep apnea and its association with pregnancy-related health outcomes: a systematic review and meta-analysis. Sleep & breathing = Schlaf & Atmung, 23(2), 399–412.
https://link.springer.com/article/10.1007/s11325-018-1714-7 -
Dunietz, G. L., Lisabeth, L. D., Shedden, K., Shamim-Uzzaman, Q. A., Bullough, A. S., Chames, M. C., Bowden, M. F., & O’Brien, L. M. (2017). Restless Legs Syndrome and Sleep-Wake Disturbances in Pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 13(7), 863–870.
https://pubmed.ncbi.nlm.nih.gov/28633715/ -
Malfertheiner, S. F., Malfertheiner, M. V., Kropf, S., Costa, S. D., & Malfertheiner, P. (2012). A prospective longitudinal cohort study: evolution of GERD symptoms during the course of pregnancy. BMC gastroenterology, 12, 131.
https://pubmed.ncbi.nlm.nih.gov/23006768/ -
Palagini, L., Gemignani, A., Banti, S., Manconi, M., Mauri, M., & Riemann, D. (2014). Chronic sleep loss during pregnancy as a determinant of stress: impact on pregnancy outcome. Sleep medicine, 15(8), 853–859.
https://linkinghub.elsevier.com/retrieve/pii/S1389945714001713 -
Gooley, J. J., Mohapatra, L., & Twan, D. (2017). The role of sleep duration and sleep disordered breathing in gestational diabetes mellitus. Neurobiology of sleep and circadian rhythms, 4, 34–43.
https://www.sciencedirect.com/science/article/pii/S2451994417300263?via%3Dihub -
Williams, M. A., Miller, R. S., Qiu, C., Cripe, S. M., Gelaye, B., & Enquobahrie, D. (2010). Associations of early pregnancy sleep duration with trimester-specific blood pressures and hypertensive disorders in pregnancy. Sleep, 33(10), 1363–1371.
https://academic.oup.com/sleep/article/33/10/1363/2454585 -
The American College of Obstetricians and Gynecologists. (2020, March). Preeclampsia and High Blood Pressure During Pregnancy., Retrieved October 16, 2020, from
https://www.acog.org/womens-health/faqs/preeclampsia-and-high-blood-pressure-during-pregnancy -
Reichner C. A. (2015). Insomnia and sleep deficiency in pregnancy. Obstetric medicine, 8(4), 168–171.
https://pubmed.ncbi.nlm.nih.gov/27512475/ -
Nakahara, K., Michikawa, T., Morokuma, S., Ogawa, M., Kato, K., Sanefuji, M., Shibata, E., Tsuji, M., Shimono, M., Kawamoto, T., Ohga, S., Kusuhara, K., & Japan Environment and Children’s Study Group (2020). Association of maternal sleep before and during pregnancy with preterm birth and early infant sleep and temperament. Scientific reports, 10(1), 11084.
https://www.nature.com/articles/s41598-020-67852-3














