Nightmare Disorder
Most people dream for about two hours each night. The purpose of dreaming is not well understood, but one theory is that it helps people to process emotions and experiences and establish memories. Dreams can be pleasurable, but they can also be sources of distress, especially when they involve frightening or disturbing scenarios.
Occasional nightmares are common among both adults and children. About 85% of adults have at least one a year, and as many as 75% of children also have nightmares. But when nightmares occur so frequently that they interfere with sleep and make it hard to function during the day, they may be indicative of a condition called nightmare disorder.
For people who have recurring nightmares, knowing when to seek help can offer a path to better sleep and improved well-being.
What Is Nightmare Disorder?
People with nightmare disorder have recurring nightmares that disrupt sleep, impair daytime functioning, and cause ongoing distress. Nightmare disorder is one of many parasomnias, which are unpleasant experiences that occur when a person is sleeping, falling asleep, or waking.
While having nightmares is the defining characteristic of nightmare disorder, not everyone who has nightmares has nightmare disorder. Nightmare disorder is also distinct from night terrors, despite their similar names.
Nightmares
Nightmares are frightening or disturbing dreams that cause the dreamer to awaken. After having nightmares, most people recall them in detail. This is because they typically happen during the rapid eye movement (REM) stage of sleep, during which brain activity resembles wakefulness.
Nightmares are often triggered by stress, a difficult life event, or trauma. Having nightmares may be a way for the brain to process anxiety and fear. Some common themes of nightmares include confrontations, chases, near-death experiences, and failure.
Given their alarming themes, nightmares can activate the nervous system’s fight-or-flight response. As a result, people may wake up from nightmares with a racing heart, feelings of panic, or sweat-soaked clothing.
Night Terrors
Unlike people with nightmares, sleepers with night terrors behave as if they are in distress, by screaming, thrashing, and even sleepwalking. While night terrors can affect adults, they are most common in children ages 3 to 7.
Night terrors occur during the sleep phase that precedes REM, known as deep sleep or slow wave sleep. While sleep terrors can resolve in minutes, some may last more than half an hour. People going through these episodes are often difficult to wake. When they do wake up, they generally have no memory of the night terror.
Nightmare Disorder
Nightmare disorder causes frequent, extended nightmares that commonly depict serious threats to the dreamer’s life, safety, and well-being. People with nightmare disorder usually have these episodes hours after falling asleep, and they wake from them feeling alert and deeply distressed. Typically, they can vividly recall the content of the nightmare.
The severity of this disorder can vary significantly. For people with mild cases, more than a week may pass between episodes. In severe cases, episodes happen nightly. Because nightmare disorder compromises sleep and creates stress, it tends to negatively affect other aspects of a person’s life, such as their ability to work.
Between 2% and 5% of adults in the U.S. experience nightmare disorder. Unfortunately, nightmare disorder is underreported and therefore undertreated. Many people do not tell their health care providers about their disruptive, frequent nightmares, and many do not know that recurring nightmares can be managed with treatment.
Risk Factors for Nightmare Disorder
According to researchers, a number of circumstances may generate nightmares or increase their frequency, putting a person at greater risk of developing nightmare disorder.
- Stress: Elevated levels of stress may cause a person to have nightmares. In some cases, a single stressful event might initiate recurring nightmares that feature distressing emotions associated with the event.
- Medications: Many medications produce nightmares as a side effect. Some blood pressure medications known as beta blockers can generate nightmares, as can certain medications for infections, depression, Parkinson’s disease, and restless legs syndrome.
- Alcohol and recreational drugs: Drinking too much alcohol or using certain recreational drugs can trigger nightmares.
- Withdrawal from substances: Nightmares can also result from ending the use of substances, including alcohol, recreational drugs, and certain prescription medications. Many medications suppress REM sleep, and when they are discontinued, the resulting rebound in REM sleep produces nightmares.
Additionally, while nightmare disorder can appear on its own, it often emerges in conjunction with other conditions and disorders .
- Posttraumatic stress disorder (PTSD): More than 70% of people with PTSD experience recurring trauma-related nightmares . In people with PTSD, nightmares may not be isolated to REM sleep but can also intrude while an individual is falling asleep.
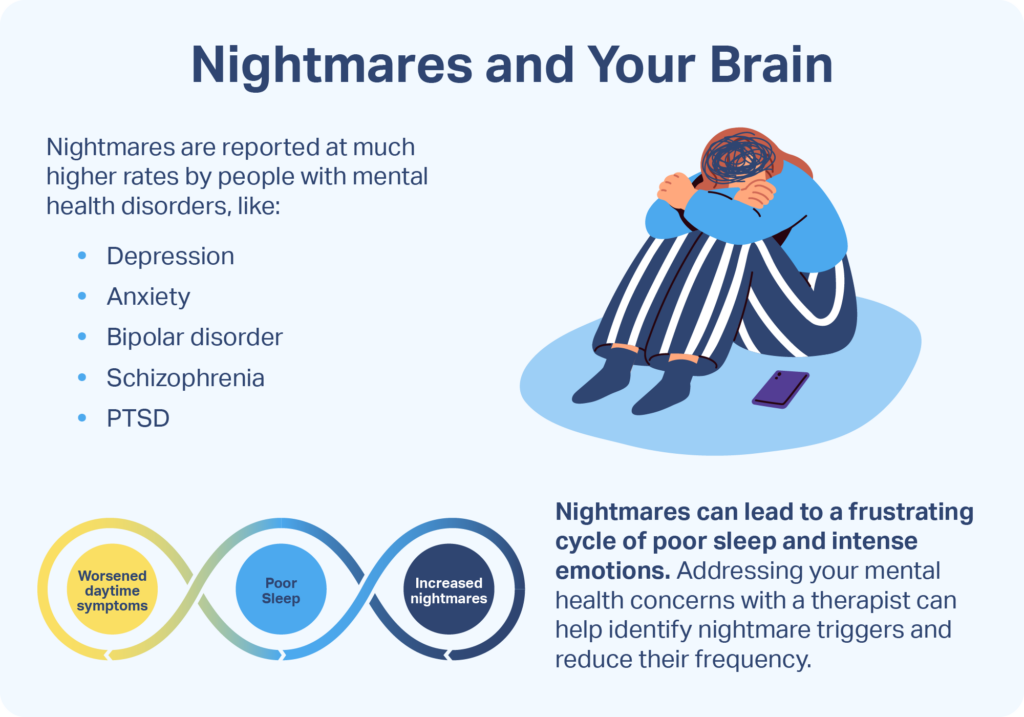
- Mental health conditions: Frequent nightmares have been linked to several mental health disorders, including depression, anxiety, schizophrenia, and borderline personality disorder. Depression, in particular, can cause changes in the sleep cycle that increase the likelihood of nightmares.
- Other sleep disorders: Nightmare disorder can occur in tandem with other sleep disorders, including insomnia, sleep apnea, and narcolepsy.

Effects of Nightmare Disorder
Nightmare disorder can affect a person’s life in many ways, both during the day and at night. The more nightmares a person has, the more susceptible they are to the physical, psychological, and social effects of nightmare disorder.
Nighttime Effects
The regular, extended nightmares resulting from nightmare disorder can have several unwelcome nighttime effects.
- Fear of falling asleep: People who dread having nightmares may develop somniphobia, the fear of falling asleep. This anxiety may cause some to delay bedtime or attempt to sleep with the lights on, behaviors that can further compromise sleep.
- Compromised sleep quantity and quality: Because nightmares cause a person to wake in a state of high alert, they decrease the amount of sleep that person is able to get. Often, people find it difficult to fall back asleep after a nightmare. When they do, their sleep can be restless and less restorative.
- Disruptions for partners and caregivers: People who wake up after having a nightmare may interrupt the sleep of their partners or caregivers. This can particularly affect the caregivers of children, who often require reassurance following a nightmare.
- Insomnia: Recurring nightmares may lead to insomnia, a sleep disorder characterized by difficulty falling and staying asleep.
Daytime Effects
The sleep disturbances and distress caused by nightmare disorder can create a number of problems during the day.
- Persistent negative emotions: Having recurring nightmares can leave people in a state of distress. In some cases, the emotions that manifest during a nightmare remain long after it has passed.
- Sleepiness: The delayed bedtimes, nighttime awakenings, and poor quality sleep associated with nightmare disorder can all contribute to daytime sleepiness and fatigue.
- Cognitive issues and impaired functioning: Following nightmares, people may have difficulty concentrating or remembering, which may affect their ability to function at home, work, or school.
Diagnosing Nightmare Disorder
A primary care physician or a sleep specialist can provide an initial diagnosis of nightmare disorder. They may ask questions about the frequency, duration, timing, and content of the nightmares, as well as how they affect the person’s sleep and life. A doctor may also gather information using a five-question diagnostic test called the nightmare disorder index.
A diagnosis of nightmare disorder may be given if a person meets these criteria :
- Recurring instances of disturbing and well-remembered nightmares in which the dreamer’s physical safety, security, or survival is at risk
- Alertness and orientation upon waking from nightmares
- Enduring feelings of distress or a compromised ability to function at home, school, work, or in one’s social life
In some situations, doctors may not diagnose nightmare disorder if they determine that a person’s nightmares are symptoms of another physical or mental health condition.
Nightmare Disorder Treatment
For some people, nightmare disorder resolves on its own over time. But for others, clinical interventions or lifestyle changes may be necessary to alleviate or eliminate recurring nightmares.
Psychotherapy
Nightmare disorder frequently occurs alongside mental health conditions like anxiety, depression, and PTSD. Treating these conditions may help to reduce the severity and frequency of nightmares and improve overall well-being. Additionally, several therapeutic approaches may be successful in directly treating nightmare disorder.
- Cognitive behavioral therapy (CBT): A common treatment for nightmare disorder, CBT can help a person understand how their thoughts and emotions might influence their nightmares, as well as how certain behaviors might contribute to or alleviate nightmares and poor sleep.
- Imagery rehearsal therapy (IRT): A variant of CBT, imagery rehearsal therapy involves creating a new script for the recurring nightmare that changes the sequence of events or the storyline into a more pleasant narrative.
- Hypnotherapy: To treat recurring nightmares, a therapist may ask a person under a highly relaxed state of hypnosis to imagine an ideal night of sleep and also offer words of encouragement, letting them know they are safe and no longer need nightmares.
- Desensitization: Desensitization helps people unlearn responses to a particular situation or stimulus. In children with nightmares, therapists may encourage desensitization by having a child write about or illustrate their nightmares.
Other possible psychotherapy treatments for nightmare disorder include sleep dynamic therapy, lucid dreaming therapy, muscle relaxation techniques, and exposure, relaxation, and rescripting therapy. Assessment by a psychiatrist or licensed mental health professional can help determine which therapeutic options may be most beneficial for a person with nightmare disorder.
Medications
Some medications, alone or in conjunction with behavioral therapy, show promise in treating nightmare disorder, although research on this topic is limited. It is best to discuss these options with a medical provider.
Wearable Technology
Preliminary evidence indicates that a smartwatch program called NightWare might improve sleep for people with PTSD-related nightmares. Authorized by the U.S. Food and Drug Administration in 2020, this product responds to physiological changes that take place during a nightmare and delivers vibrations intended to take the wearer out of REM sleep without waking them.
While early data is promising, more research is needed to validate the efficacy of this application as a treatment for nightmare disorder.
Sleep Hygiene
Some lifestyle changes that support better sleep and reduce stress may help with nightmare disorder. People with nightmare disorder may benefit from adopting practices known to promote healthy sleep, collectively called sleep hygiene. These include:
- Going to bed and waking up at the same time every day
- Establishing a bedtime routine that includes relaxing activities, such as a warm bath, gentle stretching, or listening to soothing music
- Creating a quiet and comfortable sleep environment
- Getting regular exercise earlier in the day
- Avoiding large or heavy meals before bedtime
- Avoiding screen time for at least an hour before going to bed
- Limiting or eliminating caffeine intake, alcohol consumption, and smoking in the hours before bedtime
When to Talk to Your Doctor
If you experience nightmares at least once a week, or if frequent nightmares affect your sleep, mood, or ability to function, consider speaking with a medical or mental health professional. If you suspect that recurring nightmares are caused by a new medication or could be the result of recreational drug use, make sure to mention these concerns to your provider.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
13 Sources
-
American Academy of Sleep Medicine. (2014). The International Classification of Sleep Disorders – Third Edition (ICSD-3). Darien, IL.
https://aasm.org/ -
Van Horn, N. L., & Street, M. (2022, May 30). Night terrors. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK493222/ -
Schwab, R. J. (2022, September). Overview of sleep. Merck Manual Consumer Version.
https://www.merckmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
Dietch, J. R., Taylor, D. J., Pruiksma, K., Wardle-Pinkston, S., Slavish, D. C., Messman, B., Estevez, R., Ruggero, C. J., & Kelly, K. (2021). The nightmare disorder index: Development and initial validation in a sample of nurses. Sleep, 44(5), zsaa254.
https://pubmed.ncbi.nlm.nih.gov/33245781/ -
Nadorff, M. R., Nadorff, D. K., & Germain, A. (2015). Nightmares: Under-reported, undetected, and therefore untreated. Journal of Clinical Sleep Medicine, 11(7), 747–750.
https://pubmed.ncbi.nlm.nih.gov/25845898/ -
Morgenthaler, T. I., Auerbach, S., Casey, K. R., Kristo, D., Maganti, R., Ramar, K., Zak, R., & Kartje, R. (2018). Position paper for the treatment of nightmare disorder in adults: An American Academy of Sleep Medicine position paper. Journal of Clinical Sleep Medicine, 14(6), 1041–1055.
https://pubmed.ncbi.nlm.nih.gov/29852917 -
El-Solh A. A. (2018). Management of nightmares in patients with posttraumatic stress disorder: Current perspectives. Nature and Science of Sleep, 10, 409–420.
https://pubmed.ncbi.nlm.nih.gov/30538593/ -
Cirelli, C. (2022, October 10). Insufficient sleep. In R. Benca (Ed.). UpToDate.
https://www.uptodate.com/contents/insufficient-sleep-definition-epidemiology-and-adverse-outcomes -
Paul, F., Schredl, M., & Alpers, G. W. (2015). Nightmares affect the experience of sleep quality but not sleep architecture: an ambulatory polysomnographic study. Borderline personality disorder and emotion dysregulation, 2, 3.
https://pubmed.ncbi.nlm.nih.gov/26401306/ -
Zak, R., & Karipoot, A. (2021, June 14). Nightmares and nightmare disorder in adults. In A. V. Avidan (Ed.). UpToDate.
https://www.uptodate.com/contents/nightmares-and-nightmare-disorder-in-adults -
Fariba, K. A., & Tadi, P. (2022, July 18). Parasomnias. In StatPearls. StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK560524/ -
Hauri, P. J., Silber, M. H., & Boeve, B. F. (2007). The treatment of parasomnias with hypnosis: A 5-year follow-up study. Journal of Clinical Sleep Medicine, 3(4), 369–373.
https://pubmed.ncbi.nlm.nih.gov/17694725/ -
Zagorski, N. (2020, December 14). FDA clears smartwatch app that detects, interrupts nightmares. Psychiatric News. The American Psychological Association.
https://psychnews.psychiatryonline.org/doi/10.1176/appi.pn.2020.12b15




