What Causes Insomnia?
Our medical review team has recently evaluated this page to ensure accuracy. We will continue to monitor and revise this article as new literature is published on sleepwalking.
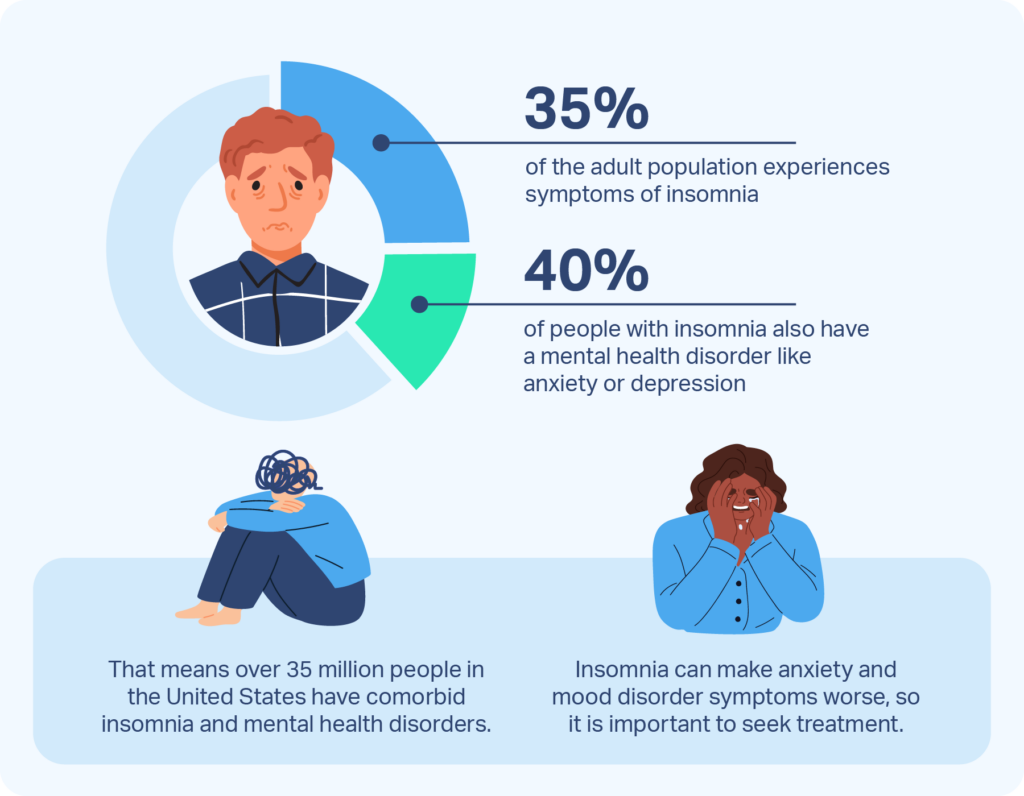
Insomnia is a sleep disorder that affects as many as 35% of adults. It is marked by problems getting to sleep, staying asleep through the night, and sleeping as long as you would like into the morning. It can have serious effects, leading to excessive daytime sleepiness, a higher risk of auto accidents, and widespread health effects from sleep deprivation.
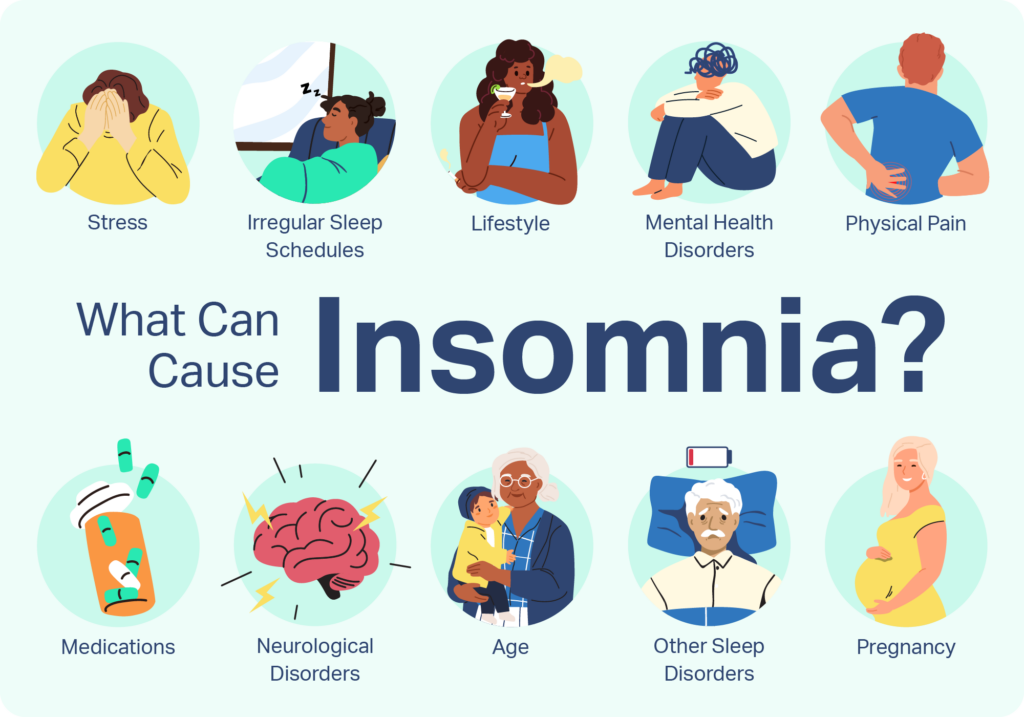
Common causes of insomnia include stress, an irregular sleep schedule, poor sleeping habits, mental health disorders, physical illnesses and pain, medications, neurological problems, and specific sleep disorders. For many people, a combination of these factors can initiate and exacerbate insomnia.
Not all insomnia is the same; people can experience the condition in distinct ways. How a person is affected by insomnia can vary significantly based on its cause, severity, and how it is influenced by underlying health conditions.
Is Your Sleep a Problem?
Insomnia is often indicative of other underlying sleep issues. Answer three questions to understand if you should be concerned.
Stress
Stress can provoke a profound reaction in the body that poses a challenge to quality sleep. This stress response can come from work, school, and social relationships. Exposure to traumatic situations can create chronic stress, including post-traumatic stress disorder (PTSD).
The body’s physical response to stress contributes to hyperarousal, and mental stress can have the same effect. The inability to sleep may itself become a source of stress, making it increasingly harder to break the cycle of stress and insomnia.
Researchers believe that some individuals are more vulnerable to stress-induced sleeping problems. These people are considered to have high “sleep reactivity,” which is tied to other issues affecting their sleep and their physical and mental health.
Irregular Sleep Schedules
In an ideal world, the body’s internal clock, known as its circadian rhythm, closely follows the daily pattern of day and night. In reality, many people have sleep schedules that cause misalignment of their circadian rhythm.
Two well-known examples are jet lag and shift work. Jet lag disturbs sleep because a person’s body can’t adjust to a rapid change in time zone. Shift work requires a person to work through the night and sleep during the day. Both can give rise to a disrupted circadian rhythm and insomnia.
In some people, circadian rhythms can be shifted forward or backward without a clear cause, resulting in persistent difficulties in sleep timing and overall sleep quality.
Lifestyle
Unhealthy habits and routines related to lifestyle and food and drink can increase a person’s risk of insomnia. Various lifestyle choices can bring about sleeping problems:
- Keeping the brain stimulated until late in the evening, such as by working late, playing video games, or using other electronic devices.
- Napping late in the afternoon can throw off your sleep timing and make it hard to fall asleep at night.
- Sleeping in later to make up for lost sleep can confuse your body’s internal clock and make it difficult to establish a healthy sleep schedule.
- Using your bed for activities besides sleep can create mental associations between your bed and wakefulness.
Though often overlooked, choices about your diet can play a role in sleeping problems like insomnia. Eating heavy meals and spicy foods can be hard on your digestive process and have the potential to generate sleeping problems when consumed later in the evening.
Caffeine is a stimulant that can stay in your system for hours, making it harder to get to sleep and potentially contributing to insomnia when used in the afternoon and evening. Nicotine is another stimulant that can negatively affect sleep.
Alcohol, which is a sedative that can make you feel sleepy, can actually worsen your sleep by disturbing your sleep cycle and causing fragmented, non-restorative sleep.
Mental Health Disorders
Mental health conditions like anxiety, depression, and bipolar disorder frequently give rise to serious sleeping problems. It is estimated that 40% of people with insomnia have a mental health disorder.
These conditions can incite pervasive negative thoughts and mental hyperarousal that disturbs sleep. In addition, poor sleep can trigger or worsen existing conditions, creating a complex chain of cause-and-effect for insomnia. Studies indicate that insomnia exacerbates mood and anxiety disorder symptoms and even increases the risk of suicide in people with depression.
Physical Illness and Pain
Almost any condition that causes pain can disrupt sleep by making it harder to lie comfortably in bed. Dwelling on pain when sleepless in bed may amplify it, increasing stress and sleeping problems. If you do suffer from pain while laying in bed, it’s important to pick the best mattress for your needs, as beds with good pressure relief can ease troublesome pain points.
Health complications related to Type II diabetes can be part of an underlying cause of insomnia. Pain from peripheral neuropathy, more frequent need for hydration and urination, and rapid blood sugar changes can interrupt sleep. There is also a correlation between diabetes and other health conditions that are known to interfere with sleep including obstructive sleep apnea (OSA) and depression.
Other types of physical illness or pain such as after a surgery, including those affecting the respiratory or nervous system, may pose challenges to sleep that can culminate in short-term or chronic insomnia.
Medications
Sleeping problems and insomnia can be side effects of many types of medications. Examples include blood pressure drugs, anti-asthma medications, and antidepressants. Other drugs may cause daytime drowsiness that can throw off a person’s sleep schedule.
It’s not just taking medications that can interrupt sleep. When someone stops taking a drug, withdrawal or other aspects of the body’s reaction can create difficulties for sleep.
Neurological Problems
Problems affecting the brain, including neurodegenerative and neurodevelopmental disorders, have been found to be associated with an elevated risk of insomnia.
Neurodegenerative disorders, such as dementia and Alzheimers dementia, can throw off a person’s circadian rhythm and perception of daily cues that drive the sleep-wake cycle. Nighttime confusion can further worsen sleep quality.
Neurodevelopmental disorders like attention-deficit/hyperactivity disorder (ADHD) can cause hyperarousal that makes it hard for people to get the sleep they need. Sleeping problems are common for children with Autism Spectrum Disorder (ASD) and may persist into adulthood.
Specific Sleep Disorders
Specific sleep disorders can be a cause of insomnia. Obstructive sleep apnea, which causes numerous breathing lapses and temporary sleep interruptions, affects up to 20% of people and can be an underlying factor causing insomnia and daytime sleepiness.
Restless legs syndrome (RLS) detracts from sleep by causing a powerful urge to move the legs. Abnormal behaviors during sleep, known as parasomnias, can interfere with sleep. Some well-known examples of parasomnias include sleepwalking, nightmares, and sleep paralysis.
Age
Stress, physical ailments, mental health problems, and poor sleep habits can cause insomnia at any age. However, teens may be especially susceptible to stress from school, work, and social obligations. Insomnia has been estimated to affect up to 23.8% of teens . Biological changes push teens toward a later, “night owl” sleep schedule, which usually does not complement school start times.
Insomnia also occurs in 30-48% of older adults . Elderly people have less sleep efficiency and are often more sensitive to symptoms of insomnia due to chronic health conditions, social isolation, and an increased use of prescription drugs. For elderly people in managed care settings, a decrease in daylight exposure can affect circadian rhythm.

Pregnancy
Multiple factors can cause insomnia during pregnancy:
- Discomfort: Increased weight and changed body composition can affect positioning and comfort in bed.
- Disrupted Breathing: Growth of the uterus places pressure on the lungs, creating potential for breathing problems during sleep. Hormonal changes can increase snoring and the risk of central sleep apnea, which involves brief lapses in breath.
- Reflux: Slower digestion can prompt disruptive gastroesophageal reflux in the evening.
- Nocturia: Greater urinary frequency can create the need to get out of bed to go to the bathroom.
- Restless Leg Syndrome: The exact cause is unknown, but pregnant women have a greater risk of RLS even if they have never had symptoms before becoming pregnant.
Studies have found that more than half of pregnant women report sleeping problems consistent with insomnia. In the first trimester, pregnant women frequently sleep more total hours, but the quality of their sleep decreases. After the first trimester, total sleep time decreases, with the most significant sleeping problems occurring during the third trimester.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
7 Sources
-
Kalmbach, D. A., Anderson, J. R., & Drake, C. L. (2018). The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. Journal of Sleep Research, 27(6), e12710.
https://pubmed.ncbi.nlm.nih.gov/29797753/ -
Schwab, R. J. (2020a, June). MSD Manual Consumer Version: Insomnia and Excessive Daytime Sleepiness (EDS)., Retrieved July 20, 2020.
https://www.msdmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/insomnia-and-excessive-daytime-sleepiness-eds -
Resnick, H. E., Redline, S., Shahar, E., Gilpin, A., Newman, A., Walter, R., Ewy, G. A., Howard, B. V., Punjabi, N. M., & Sleep Heart Health Study (2003). Diabetes and sleep disturbances: findings from the Sleep Heart Health Study. Diabetes care, 26(3), 702–709.
https://diabetesjournals.org/care/article/26/3/702/29232/Diabetes-and-Sleep-DisturbancesFindings-from-the -
Franklin, K. A., & Lindberg, E. (2015). Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. Journal of thoracic disease, 7(8), 1311–1322.
https://pubmed.ncbi.nlm.nih.gov/26380759/ -
Donskoy, I., & Loghmanee, D. (2018). Insomnia in Adolescence. Medical sciences (Basel, Switzerland), 6(3), 72.
https://pubmed.ncbi.nlm.nih.gov/30200388/ -
Patel, D., Steinberg, J., & Patel, P. (2018). Insomnia in the Elderly: A Review. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 14(6), 1017–1024.
https://pubmed.ncbi.nlm.nih.gov/29852897/ -
Kızılırmak, A., Timur, S., & Kartal, B. (2012). Insomnia in pregnancy and factors related to insomnia. TheScientificWorldJournal, 2012, 197093.
https://pubmed.ncbi.nlm.nih.gov/22623880/























