What is NREM Sleep?
- Non-rapid eye movement (NREM) sleep is an essential part of the sleep cycle.
- It involves three stages: N1, N2, and N3, with N3 being the deepest.
- NREM sleep stages are vital for physical and mental restoration.
- Sleep deprivation and fragmented sleep can limit your amount of time spent in NREM sleep and lead to health problems.
We tend to think of sleep as a time of rest, but in reality it is a highly active process. Experts divide sleep into four stages of rapid eye movement (REM) and non-rapid eye movement (NREM) sleep. Each stage plays an important role in repairing and rebuilding the brain and body. Throughout the night, you cycle multiple times through all four sleep stages. A complete cycle takes approximately 90 minutes.
REM sleep is the stage most people associate with dreaming, although it is also possible to dream during NREM sleep. The other three stages of sleep are collectively referred to as NREM sleep. Experts are still investigating why we divide sleep into NREM and REM sleep, and whether these two types of sleep exist independently or whether they work in tandem.
NREM sleep appears to occur in virtually all animals. Most people spend more time in NREM sleep in the first half of the night, for a total of 75% to 80% in NREM sleep over the whole sleep period. We’ll take a closer look at the purpose of NREM sleep and its different components.
What Is NREM Sleep?
Non-rapid eye movement (NREM) sleep encompasses three sleep stages , referred to as stage 1, stage 2, and stage 3 NREM sleep. While unique mental processes characterize each stage, they share a tendency for the sleeper to experience slowed breathing, muscle activity, heartbeat, and brain waves. NREM sleep is differentiated from rapid eye movement (REM) sleep because sleepers experience slowed eye movements during NREM sleep.
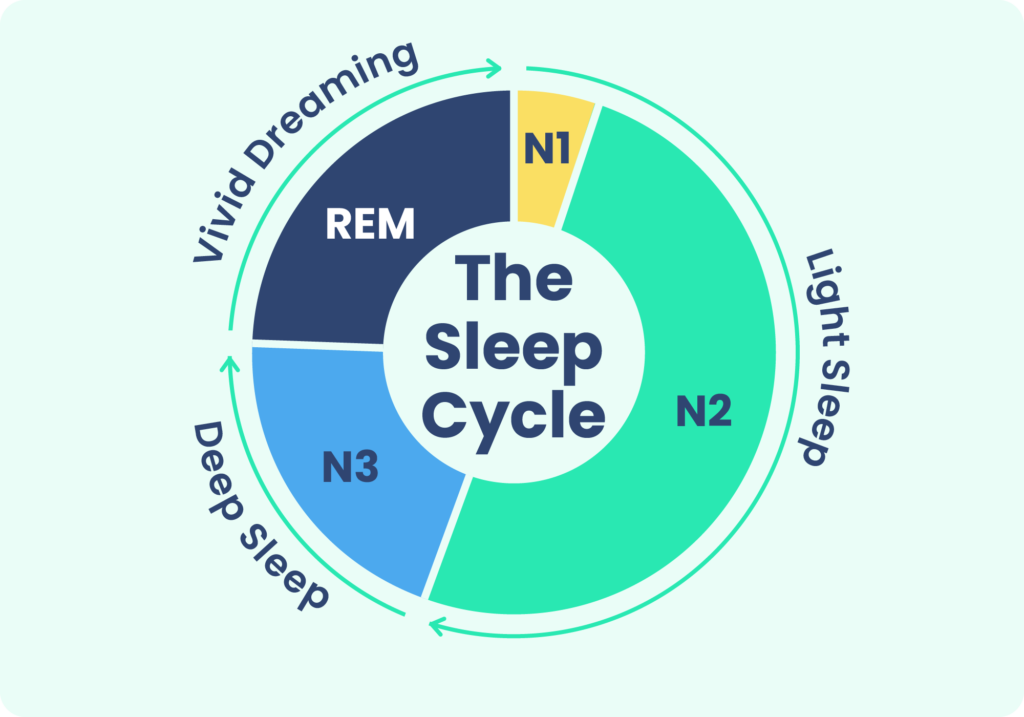
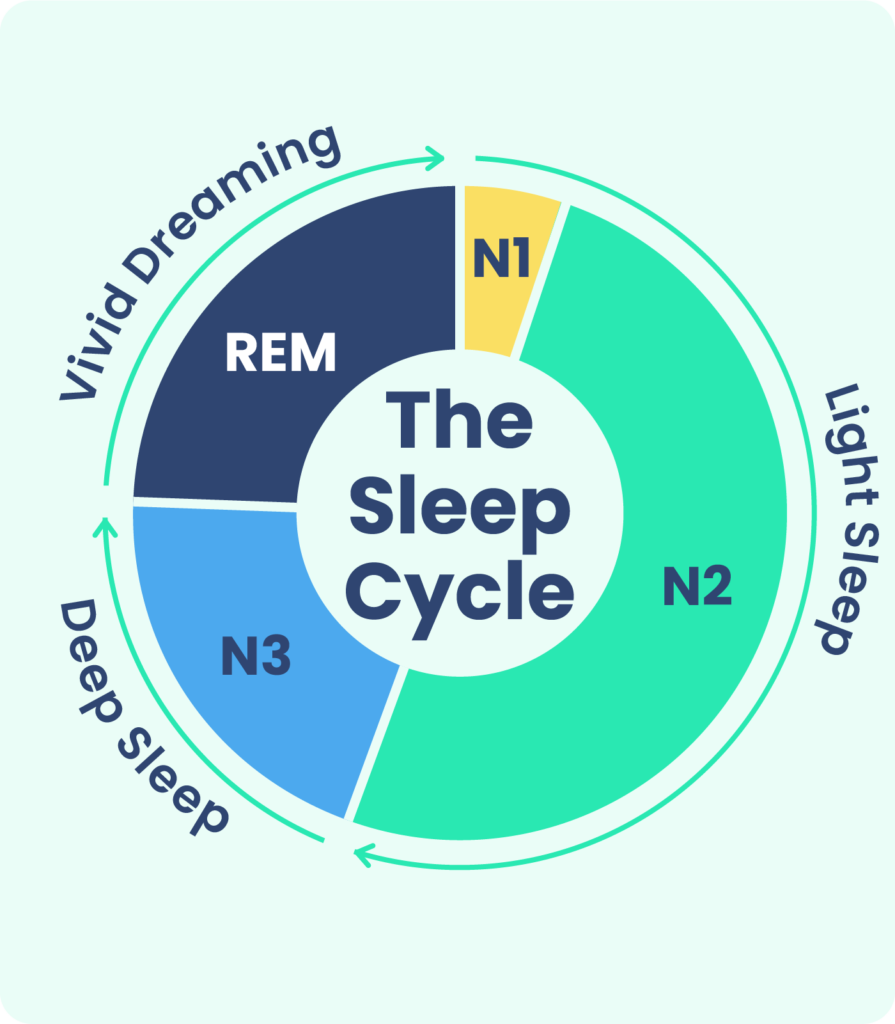
Stage 1 and stage 2 NREM sleep are considered light sleep, while stage 3 NREM sleep is considered deep sleep. Certain hallmarks of electrical activity in the brain appear during each stage. These are usually described by their frequency, or Hertz. A higher number indicates that neurons are firing more rapidly.
What Happens During NREM Sleep?
As you cycle through stage 1, stage 2, and then stage 3 NREM sleep, various bodily functions slow down or stop altogether, allowing reparative and restorative processes to take over.
Stage 1
Stage 1 NREM sleep is the first sleep stage you enter when nodding off. This sleep stage is when heartbeat, eye movements, brain waves, and breathing activity begin to taper down. Motor movements also diminish, although you may experience muscle twitches called hypnic jerks. The first episode of stage 1 sleep usually only lasts a few minutes.

Stage 2
Stage 2 NREM sleep sees a continued slowing of heartbeat, breathing, muscle activity, and eye movements. During this stage, you also experience a reduction in body temperature. Throughout the course of the night, you spend about half the time in stage 2 sleep .
Brain waves generally slow further during stage 2 sleep. However, this sleep stage is also marked by the appearance of two unique types of brain activity:
Sleep Spindles
Sleep spindles are short bursts of brain activity lasting 0.5 to three seconds. Occurring every three to six seconds during stage 2 sleep and occasionally during other stages sleep spindles are essential for memory and learning. They likely also help shut out external stimuli so you do not wake up as easily. Sleep spindles have a frequency of approximately 7 to 15 Hertz and can be classified into two categories: slow or fast , representing activity in different areas of the brain.
K-Complexes
K-complexes consist of a single sharp peak in electrical activity, followed immediately by a negative dip. Like sleep spindles, K-complexes may play a role in maintaining sleep by blocking out reactions to harmless sounds and lights. Somewhat paradoxically, K-complexes may also help wake you up if the brain perceives a stimulus as dangerous. K-complexes are thought to contribute to memory consolidation and neural maintenance to keep the brain running smoothly.
Stage 3
Your heartbeat, breathing, muscle activity, and brain waves are at their slowest during stage 3 sleep. This sleep stage is otherwise known as deep sleep, because experts believe it to be the most critical stage for regenerating your body and brain.
The body releases growth hormone during this stage and carries out tissue, muscle, and bone repair. Researchers believe deep sleep helps regulate glucose metabolism, immune system functioning, hormone release, and memory.
The majority of brain waves during stage 3 NREM sleep are called delta waves. These are large waves with a relatively slow frequency of 1 to 4 Hertz. Stage 3 NREM sleep also displays so-called slow oscillations, which are even slower at 0.5 to 1 Hertz. Slow oscillations may help synchronize delta waves and spindle waves, which can also occur during deep sleep.
Together, delta waves and slow oscillations are referred to as slow wave activity, and this sleep stage is often called slow wave sleep.
People are less receptive to outside stimuli during deep sleep, so it can be difficult to awaken them. If you do manage to wake someone out of deep sleep, they may experience a period of grogginess called sleep inertia.
Most people obtain the bulk of their deep sleep at the beginning of the night. Without enough slow wave sleep, you can wake up feeling unrefreshed. Thus, after a period of sleep deprivation, you compensate by reducing spindle activity and spending more time in deep sleep during the next sleep period. Deep sleep decreases across the lifespan, with young children obtaining more deep sleep and older adults typically receiving less deep sleep.
Why Is NREM Sleep Important?
NREM has been primarily studied for its contributions to physical recovery and memory consolidation. Researchers have proposed that abnormalities in NREM sleep processes may play a role in schizophrenia , epilepsy , Alzheimer’s and Parkinson’s disease , and autism spectrum disorders .
Physical Growth and Repair
Traditionally, NREM sleep has been viewed as a time of rest. In support of this theory, researchers have found that the brain uses significantly less energy during NREM sleep. By contrast, during NREM sleep, people with insomnia display brain waves that are similar to wakefulness. They also maintain a faster metabolism and heart rate , indicating they are unable to fully relax. Sleep disruption for other reasons can also interfere with the restorative process.
Studies have found that sleep disorders that interrupt sleep may interfere with fat metabolism, which in turn impacts levels of growth hormone, leading to a vicious cycle and further problems with fat metabolism.
NREM sleep may also impact the cardiovascular system. During slow wave sleep in particular, blood pressure drops , which is thought to play a protective role against heart disease. People with conditions such as sleep apnea, chronic insomnia, high blood pressure, or those who experience interrupted sleep may not experience this dip in blood pressure, which can raise the risk of heart problems.
Memory Consolidation
During NREM sleep, the brain consolidates new memories and skills into a more durable format. It also optimizes mental pathways for future learning. Specific patterns during NREM sleep are associated with better working memory, verbal fluency, motor learning, and word retrieval. People who show higher proportions of alternate patterns do not perform as well on these variables.
NREM sleep is thought to play a role in both declarative and procedural memory . Declarative memory is the ability to recall information, such as naming the 50 states. Procedural memory is the ability to learn new tasks, such as playing the violin.
One theory is that sleep spindles help strengthen neural connections related to recently acquired memories, and then slow wave sleep tidies up the pathways so they are ready for use the next day. In older adults, slow waves and spindles do not synchronize as well, which may explain memory problems as people age .
The contribution of slow wave sleep to the optimization of these pathways can be conceived as a recovery period from the day’s learning. Researchers propose that more slow wave sleep is needed to recover after either more time spent awake, or a more intensive learning process.
Along the same lines, it makes sense that as you spend less time in deep sleep once you reach adulthood, you are less able to learn new skills. Between the ages of 10 and 20, slow wave sleep gradually diminishes by more than 60% .
Fast and slow spindles represent activity in different brain regions, and researchers believe transitions in spindle activity might represent the maturation of the brain . Overall, spindle activity grows during childhood and adolescence, peaks in early adulthood, and drops off again. During adolescence, fast spindles may play a role in memory consolidation, whereas slow spindles are more related to general cognitive ability.
When to Talk to Your Doctor
Sleep deprivation can cause chronic health problems down the line, so it is important to monitor any changes to your sleep and wake patterns and aim for the recommended sleep times according to your age group.
If you are having trouble sleeping and you do not know why, ask your doctor. They can recommend sleep hygiene tips to help you sleep better, and they may be able to identify an underlying sleep disorder that could be interfering with NREM sleep.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
20 Sources
-
Schwab, R.J. (2020, June). Overview of sleep. Merck Manual Professional Version., Retrieved November 28, 2021, from
https://www.msdmanuals.com/home/brain,-spinal-cord,-and-nerve-disorders/sleep-disorders/overview-of-sleep -
Le Bon O. (2020). Relationships between REM and NREM in the NREM-REM sleep cycle: A review on competing concepts. Sleep Medicine, 70, 6–16.
https://pubmed.ncbi.nlm.nih.gov/32179430/ -
Patel, A. K., Reddy V., Araujo J. F. (2019, March). Physiology, sleep stages. StatPearls.
https://pubmed.ncbi.nlm.nih.gov/30252388/ -
Alfonsi, V., D’Atri, A., Gorgoni, M., Scarpelli, S., Mangiaruga, A., Ferrara, M., & De Gennaro, L. (2019). Spatiotemporal dynamics of sleep spindle sources across NREM sleep cycles. Frontiers in Neuroscience, 13, 727.
https://pubmed.ncbi.nlm.nih.gov/31354426/ -
Gandhi, M. H., & Emmady, P. D. (2021). Physiology, K complex. In StatPearls. StatPearls Publishing.
https://pubmed.ncbi.nlm.nih.gov/32491401/ -
Xu, H., Xia, Y., Li, X., Qian, Y., Zou, J., Fang, F., Yi, H., Wu, H., Guan, J., & Yin, S. (2020). Association between obstructive sleep apnea and lipid metabolism during REM and NREM sleep. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 16(4), 475–482.
https://pubmed.ncbi.nlm.nih.gov/32003732/ -
Léger, D., Debellemaniere, E., Rabat, A., Bayon, V., Benchenane, K., & Chennaoui, M. (2018). Slow-wave sleep: From the cell to the clinic. Sleep Medicine Reviews, 41, 113–132.
https://pubmed.ncbi.nlm.nih.gov/29490885/ -
Gaudreau, H., Carrier, J., & Montplaisir, J. (2001). Age-related modifications of NREM sleep EEG: From childhood to middle age. Journal of Sleep Research, 10(3), 165–172.
https://pubmed.ncbi.nlm.nih.gov/11696069/ -
Feinberg, I., de Bie, E., Davis, N. M., & Campbell, I. G. (2011). Topographic differences in the adolescent maturation of the slow wave EEG during NREM sleep. Sleep, 34(3), 325–333.
https://pubmed.ncbi.nlm.nih.gov/21358849/ -
Schmitt B. (2015). Sleep and epilepsy syndromes. Neuropediatrics, 46(3), 171–180.
https://pubmed.ncbi.nlm.nih.gov/25965811/ -
Lucey, B. P., McCullough, A., Landsness, E. C., Toedebusch, C. D., McLeland, J. S., Zaza, A. M., Fagan, A. M., McCue, L., Xiong, C., Morris, J. C., Benzinger, T., & Holtzman, D. M. (2019). Reduced non-rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Science Translational Medicine, 11(474), Article eaau6550.
https://pubmed.ncbi.nlm.nih.gov/30626715/ -
Priano, L., Bigoni, M., Albani, G., Sellitti, L., Giacomotti, E., Picconi, R., Cremascoli, R., Zibetti, M., Lopiano, L., & Mauro, A. (2019). Sleep microstructure in Parkinson’s disease: Cycling alternating pattern (CAP) as a sensitive marker of early NREM sleep instability. Sleep Medicine, 61, 57–62.
https://pubmed.ncbi.nlm.nih.gov/31307885/ -
Rochette, A. C., Soulières, I., Berthiaume, C., & Godbout, R. (2018). NREM sleep EEG activity and procedural memory: A comparison between young neurotypical and autistic adults without sleep complaints. Autism Research: Official Journal of the International Society for Autism Research, 11(4), 613–623.
https://pubmed.ncbi.nlm.nih.gov/29381247/ -
Wu, Y. M., Pietrone, R., Cashmere, J. D., Begley, A., Miewald, J. M., Germain, A., & Buysse, D. J. (2013). EEG power during waking and NREM sleep in primary insomnia. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine, 9(10), 1031–1037.
https://pubmed.ncbi.nlm.nih.gov/24127147/ -
Huang, Z., Goparaju, B., Chen, H., & Bianchi, M. T. (2018). Heart rate phenotypes and clinical correlates in a large cohort of adults without sleep apnea. Nature and Science of Sleep, 10, 111–125.
https://pubmed.ncbi.nlm.nih.gov/29719424/ -
Vahdat, S., Fogel, S., Benali, H., & Doyon, J. (2017). Network-wide reorganization of procedural memory during NREM sleep revealed by fMRI. eLife, 6, Article e24987.
https://pubmed.ncbi.nlm.nih.gov/28892464/ -
Siclari, F., Bernardi, G., Cataldi, J., & Tononi, G. (2018). Dreaming in NREM sleep: A high-density EEG study of slow waves and spindles. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, 38(43), 9175–9185.
https://pubmed.ncbi.nlm.nih.gov/30201768/ -
Helfrich, R. F., Mander, B. A., Jagust, W. J., Knight, R. T., & Walker, M. P. (2018). Old brains come uncoupled in sleep: Slow wave-spindle synchrony, brain atrophy, and forgetting. Neuron, 97(1), 221–230.e4.
https://pubmed.ncbi.nlm.nih.gov/29249289/ -
Campbell, I. G., Darchia, N., Higgins, L. M., Dykan, I. V., Davis, N. M., de Bie, E., & Feinberg, I. (2011). Adolescent changes in homeostatic regulation of EEG activity in the delta and theta frequency bands during NREM sleep. Sleep, 34(1), 83–91.
https://pubmed.ncbi.nlm.nih.gov/21203377/ -
Hahn, M., Joechner, A. K., Roell, J., Schabus, M., Heib, D. P., Gruber, G., Peigneux, P., & Hoedlmoser, K. (2019). Developmental changes of sleep spindles and their impact on sleep-dependent memory consolidation and general cognitive abilities: A longitudinal approach. Developmental Science, 22(1), Article e12706.
https://pubmed.ncbi.nlm.nih.gov/30252185/








