How Can Menopause Affect Sleep
If you are over the age of 40 and have trouble sleeping, wake up hot and sweaty, or feel tired during the day, you are not alone. Menopause, the time in life when a person’s periods stop for 12 consecutive months, brings about a series of changes—including shifts in sleep patterns.
As many as 46% of individuals have sleep difficulties in the years leading up to menopause. Following menopause, about half of people experience sleep disorders. Understanding the intersection of menopause and sleep is crucial for those navigating this transformative period.
Are You Getting Enough Deep Sleep?
A variety of issues can cause degrade your sleep quality. Answer three questions to understand if it’s a concern you should worry about.
Sleep Problems Associated With Menopause
The symptoms of menopause usually begin about four to seven plus years before a person’s last period and can continue for years afterward. The hormonal shifts, physical changes, and life circumstances that happen during this time can contribute to several different sleep problems.
Hot Flashes and Night Sweats
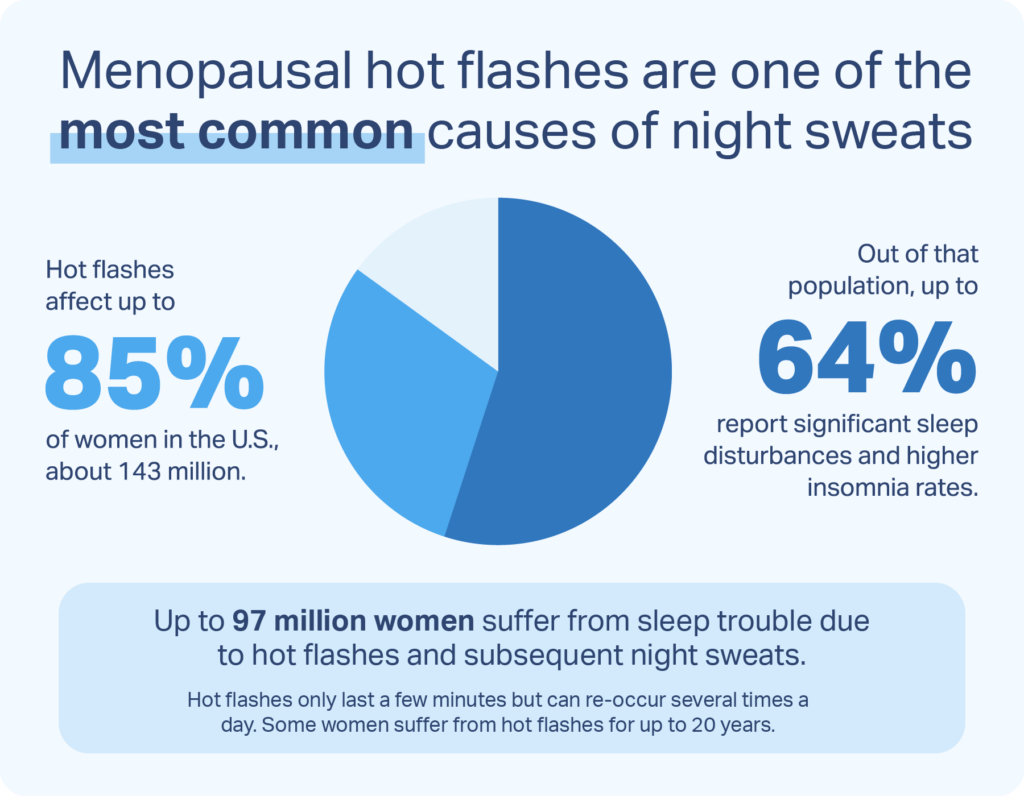
Most people going through menopause experience hot flashes, episodes of intense heat that spread from the chest up. Hot flashes—or “night sweats,” as they are called at night—usually last two to four minutes and are often accompanied by profuse sweating and feelings of anxiety.
When someone wakes up during a hot flash, the discomfort and agitation they feel can make it harder to fall back asleep. Night sweats tend to become more frequent as a person nears menopause and may continue to occur often and at high intensity in the years immediately following their last period.
Insomnia
During and after the menopausal transition, people have an increased risk of developing insomnia, a sleep disorder characterized by difficulty falling and staying asleep. Despite the long-held belief that night sweats lead to insomnia, research suggests that increased wakefulness causes people to notice and feel bothered by hot flashes that they might otherwise sleep through.
The prevalence of insomnia during the menopausal transition may be linked to anxiety and depression. Hormonal changes and life circumstances—such as divorce or caring for aging parents—can contribute to declining mental health in the years before and after menopause, and most people with depression or anxiety experience chronic insomnia.
Snoring and Sleep Apnea
During the menopausal transition and after menopause, snoring becomes increasingly common. Declining reproductive hormones can cause the soft tissues in the throat to become more collapsible, and the weight gain that commonly occurs during menopause can cause obstructions in the airway. The snoring that results can disrupt sleep.
Snoring can also be a symptom of sleep apnea, a sleep disorder that causes breathing to become shallow or to stop altogether for short periods of time. These breathing events can reduce sleep quality, lead to daytime sleepiness, and potentially contribute to long-term physical and mental health problems. Sleep apnea affects about a quarter of people in the years leading up to menopause and more than a third in the years that follow. If you have symptoms of sleep apnea, including snoring, waking up choking or gasping for air, or morning headaches, taking a home sleep test is highly recommended.
Restless Legs Syndrome
More than half of post-menopausal people experience restless legs syndrome (RLS), a sleep disorder that causes uncomfortable sensations in the legs when lying down. This discomfort is typically relieved by movement—but only temporarily, which can make it difficult to sleep and may lead to insomnia. Experts hypothesize that fluctuating hormones, as well as iron deficiency, may trigger RLS following menopause.

Why Does Menopause Affect Sleep?
During the menopausal transition, the body produces increasingly less estrogen and progesterone, hormones involved in the reproductive cycle. These changes affect many systems and processes in the body, including several that impact sleep.
- Thermoregulation: During menopause, estrogen withdrawal causes the brain to become more reactive to temperature shifts. This causes it to initiate cooling processes, like sweating, at lower core body temperatures—leading to hot flashes and night sweats.
- Mood: Changing estrogen levels may interfere with neurotransmitters involved in mood regulation. This could explain why mood swings, depression, and anxiety are more prevalent during the menopausal transition—along with the sleep difficulties associated with these conditions.
- Metabolism: Menopause affects the way the body converts food into energy. Low estrogen levels can contribute to weight gain, which in turn, can contribute to the development of snoring or sleep apnea.
- Circadian Rhythm: Following menopause, many people experience a weakening of their circadian rhythms, the biological processes that operate according to a 24-hour clock. This includes the sleep-wake cycle.
The Role Your Hormones Can Play
Because the hormonal changes that occur during menopause cause most of its unpleasant side-effects, menopausal hormone therapy (MHT) is one of the primary treatments used to alleviate the symptoms of menopause. Research shows that MHT, also sometimes called hormone replacement therapy (HRT), can effectively reduce:
- Night sweats
- Mood swings and depression
- Sleep difficulties
Generally, MHT involves boosting estrogen levels, which can be done with a pill, skin patch, or gel. People who take estrogen and still have their uteruses must also take synthetic progesterone, usually in the form of a pill, to prevent irregular thickening of their uteruses. Additionally, research suggests that taking synthetic progesterone alone can improve hot flashes and night sweats.
Some evidence indicates that taking melatonin—a sleep hormone—can improve sleep during and after the menopausal transition. Taking melatonin supplements may also elevate mood and reduce hot flashes.
Managing Menopause, Improving Sleep: How To Do Both
In addition to hormone therapy, there are several steps you can take to manage the symptoms of menopause and support healthy, restorative sleep.
- Optimize your sleep environment: Make sure your bedroom is cool, dark, and quiet. Run a fan, if you have one, and keep a glass of ice water nearby.
- Manage stress: Consider incorporating stress-reduction techniques, such as mindfulness meditation, into your bedtime routine.
- Commit to a healthy diet: Eat a plant-based diet that is low in fats, high in antioxidants, and rich in calcium and vitamin D.
- Avoid alcohol, caffeine, and tobacco: These substances can all interfere with sleep and intensify hot flashes.
- Exercise regularly: In addition to helping you sleep better, regular exercise supports heart health, prevents the loss of bone and muscle mass, and helps reduce stress.
- Try cognitive behavioral therapy for insomnia (CBT-I): This first-line treatment for insomnia can help with menopause-related sleep problems and reduce the feelings of irritation that accompany hot flashes.
Some of the sleep disorders and mental health conditions that are prevalent in menopause require treatment by a medical professional. If you suspect you have sleep apnea, restless legs syndrome, depression, or anxiety, talk to your doctor.
If you don’t have a doctor, Midi Health is a virtual care clinic focused on women navigating perimenopause and menopause. Along with helping you navigate sleep issues, Midi’s trained clinicians provide patients with personalized care for hot flashes and night sweats, moodiness, anxiety, brain fog, weight gain, and many more symptoms of hormonal change. Treatments may include hormonal and non-hormonal medications, supplements, and lifestyle coaching and Midi’s care is guided by world-class experts in women’s midlife health.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
10 Sources
-
Casper, R. (2023 December). Clinical manifestations and diagnosis of menopause. In R. Barbieri, W. Crowley, & K. Martin (Ed.). UpToDate.
https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-menopause -
Bianchi, M. T., Kim, S., Galvan, T., White, D. P., & Joffe, H. (2016). Nocturnal Hot Flashes: Relationship to Objective Awakenings and Sleep Stage Transitions. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 12(7), 1003–1009.
https://pubmed.ncbi.nlm.nih.gov/26951410 -
Alblooshi, S., Taylor, M., & Gill, N. (2023). Does menopause elevate the risk for developing depression and anxiety? Results from a systematic review. Australasian psychiatry : bulletin of Royal Australian and New Zealand College of Psychiatrists, 31(2), 165–173.
https://pubmed.ncbi.nlm.nih.gov/36961547 -
Salari, N., Hasheminezhad, R., Hosseinian-Far, A., Rasoulpoor, S., Assefi, M., Nankali, S., Nankali, A., & Mohammadi, M. (2023). Global prevalence of sleep disorders during menopause: a meta-analysis. Sleep & breathing = Schlaf & Atmung, 27(5), 1883–1897.
https://pubmed.ncbi.nlm.nih.gov/36892796 -
Saaresranta, T., Anttalainen, U., & Polo, O. (2015). Sleep disordered breathing: is it different for females?. ERJ open research, 1(2), 00063-2015.
https://pubmed.ncbi.nlm.nih.gov/27730159 -
Mirer, A. G., Young, T., Palta, M., Benca, R. M., Rasmuson, A., & Peppard, P. E. (2017). Sleep-disordered breathing and the menopausal transition among participants in the Sleep in Midlife Women Study. Menopause (New York, N.Y.), 24(2), 157–162.
https://pubmed.ncbi.nlm.nih.gov/27760083/ -
Seeman M. V. (2020). Why Are Women Prone to Restless Legs Syndrome?. International journal of environmental research and public health, 17(1), 368.
https://pubmed.ncbi.nlm.nih.gov/31935805 -
Martin, K. & Barbieri, R. (2023 December). Treatment of menopausal symptoms with hormone therapy. In W. Crowley & J. Mulder. UpToDate
https://www.uptodate.com/contents/treatment-of-menopausal-symptoms-with-hormone-therapy -
Dolitsky, S. N., Cordeiro Mitchell, C. N., Stadler, S. S., & Segars, J. H. (2020). Efficacy of progestin-only treatment for the management of menopausal symptoms: a systematic review. Menopause (New York, N.Y.), 28(2), 217–224.
https://pubmed.ncbi.nlm.nih.gov/33109992/ -
Parandavar, N., Abdali, K., Keshtgar, S., Emamghoreishi, M., & Amooee, S. (2014). The Effect of Melatonin on Climacteric Symptoms in Menopausal Women; A Double-Blind, Randomized Controlled, Clinical Trial. Iranian journal of public health, 43(10), 1405–1416.
https://pubmed.ncbi.nlm.nih.gov/26060703












