Painsomnia Steals 51.5 Minutes of Our Sleep Every Night. How Do We Cope?
- Painsomnia, or insomnia from chronic pain, affects a large number of U.S. adults.
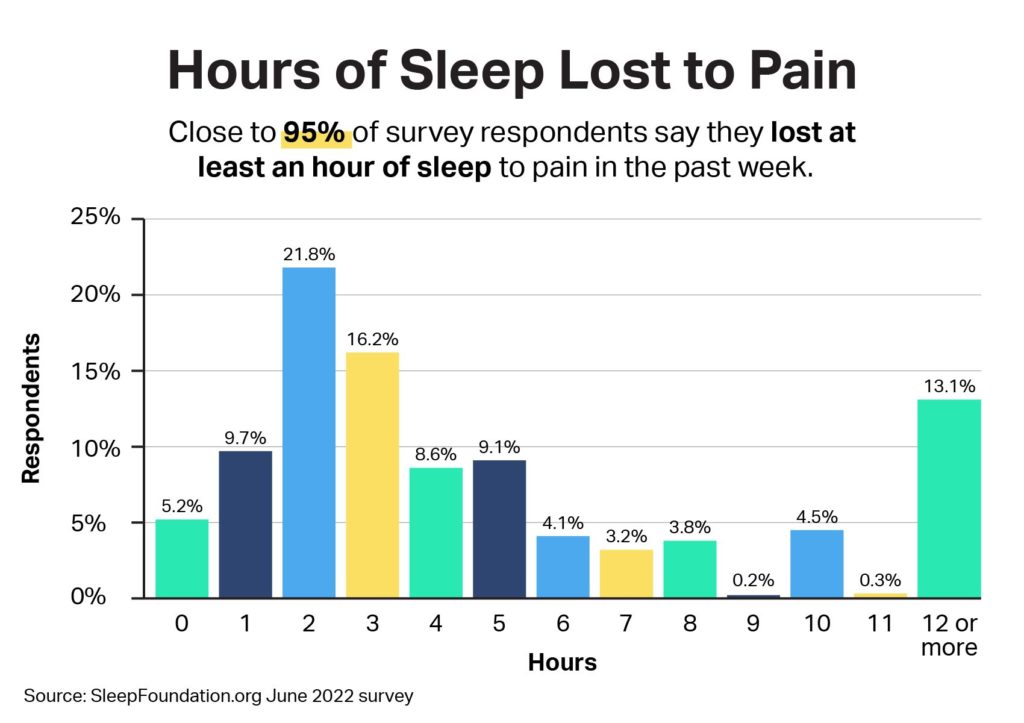
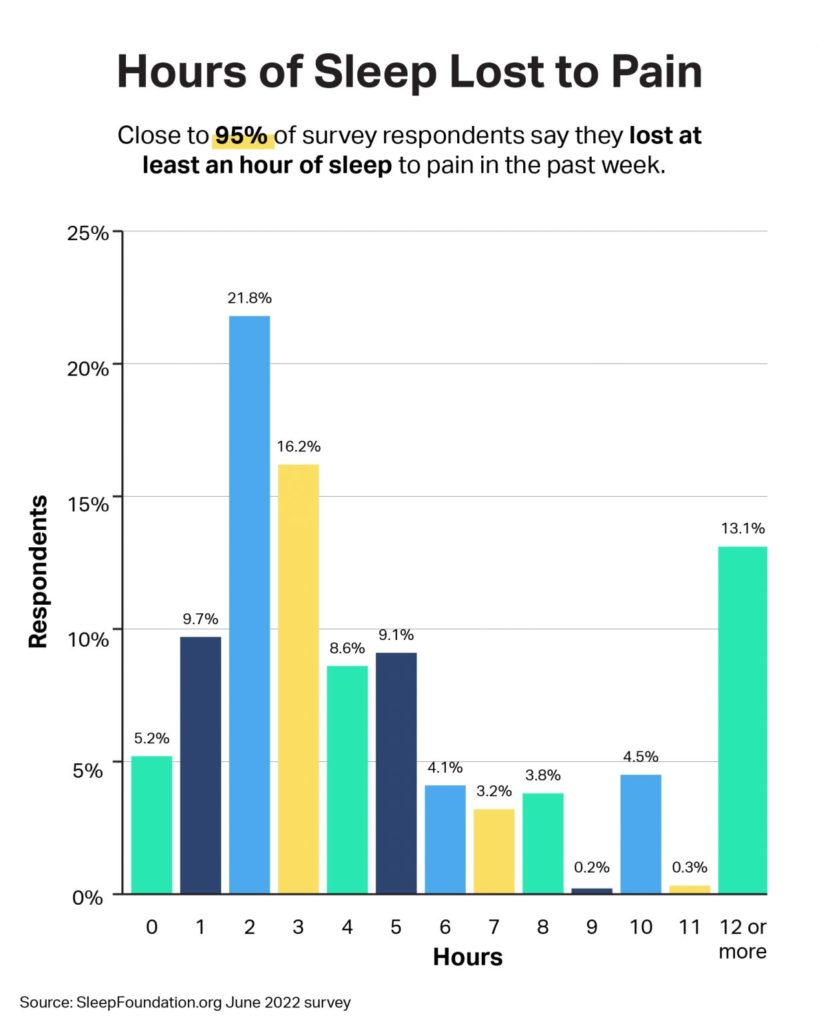
- 94.8% of adults lost at least an hour of sleep to pain in the past week.
- 85.1% of adults lost at least two hours of sleep to pain each night.
- On average, pain costs adults 51.5 minutes of sleep every night.
- People who experience pain at least one night a week average 6.7 hours of sleep.
- 57% of people who experience regular pain wake up at least three times during the night
- Back pain was the most common ailment among painsomniacs, accounting for 56.2% of adults who lost sleep to pain.
An ankle injury 10 years ago keeps JC Drake awake even today. It’s a condition loosely known as painsomnia, or insomnia from chronic pain, and it’s a regular reality for the 48-year-old resident of Germantown, Maryland. Daily pain makes a good night’s sleep challenging. And Drake is not alone.
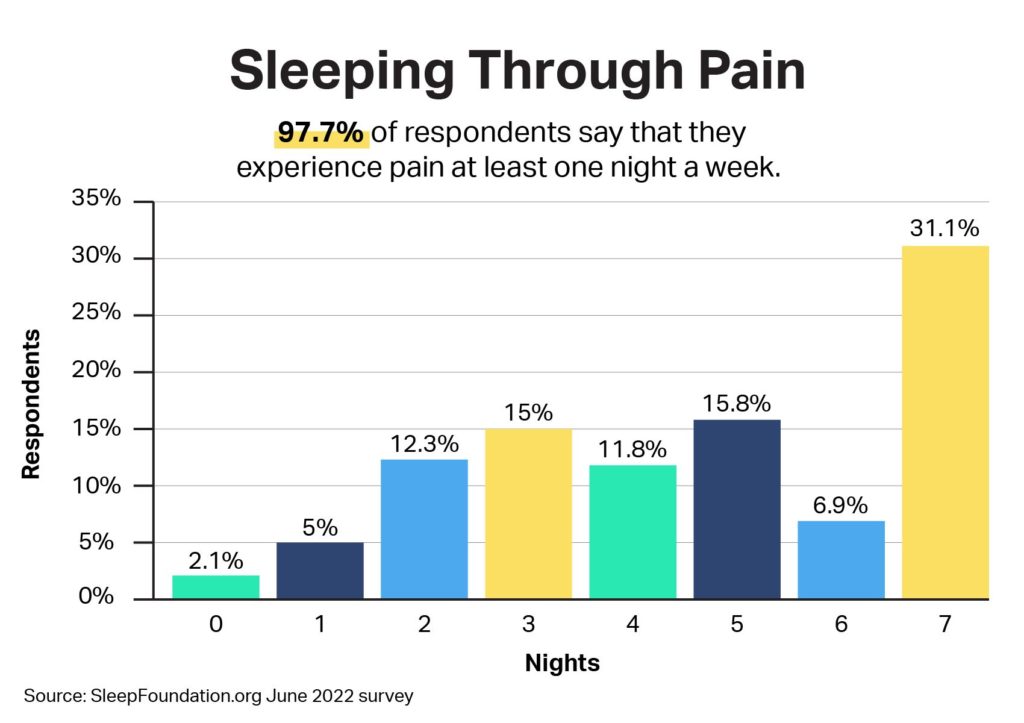
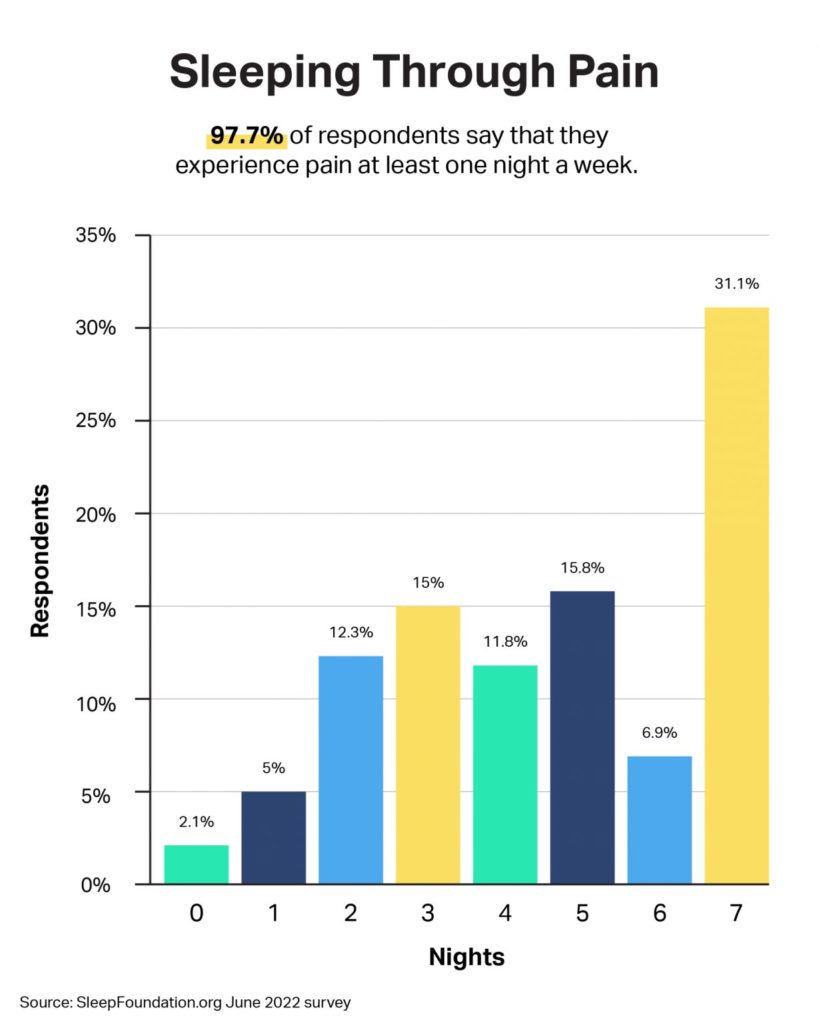
According to a SleepFoundation.org June 2022 survey of 1,250 U.S. adults, 94.8% of people say they have lost at least an hour of sleep to pain in total in the past week. The vast majority, 85.1%, say that pain costs them at least two hours of sleep each night.
On average, respondents say they are losing six hours of sleep per week to pain. That means that pain is costing us nearly an hour of sleep, or 51.5 minutes, each night.
Adults who have pain average 6.7 hours of sleep per night, below the recommended seven to nine hours. This is also below or in line with prior sleep polls , which found that people who experience pain sleep 6.7 to seven hours nightly, depending on pain severity.
How many people experience chronic pain? In the United States, it’s 25.4% of adults, according to research published in 2021. The Centers for Disease Control and Prevention note a higher prevalence among women (21.4%) and white adults (23.6%) versus Black (19.3%), Latino (13%), and Asian adults (6.8%).
Diving deeper into these findings, we can get a greater sense of who is experiencing painsomnia, as well as the communities emerging online to help address it.

What Is Painsomnia?
Painsomnia is not a specific medical term. But researchers have long documented the connection between insomnia and pain .
Insomnia is a diagnosed condition in which trouble falling or staying asleep leads to impairment during the day. Pain has a similar impairing effect.
“Chronic pain and insomnia go hand in hand, unless the pain is well-managed,” says Dr. Medhat Mikhael, pain management specialist and medical director of the Spine Health Center at MemorialCare Orange Coast Medical Center in Fountain Valley, California.
That said, pain and insomnia may co-exist without a diagnosis of either. Among people who reported feeling pain that kept them up at least one night a week, 40.3% say they have not been diagnosed with a sleep disorder. About one-third, or 32.7%, have received an insomnia diagnosis, with 23.8% also saying they have received a diagnosis of sleep apnea and 21% having restless legs syndrome.
Regardless of diagnosis, there are a few ways pain affects sleep. First, it increases latency, or the time it takes to fall asleep. People with pain toss and turn a lot before sleeping, Dr. Mikhael says. Among surveyed U.S. adults, 54.4% reported that pain kept them from falling asleep.
The connection between sleep problems and pain is bidirectional, too. A The September 2022 meta-analysis of 31 studies found that sleep loss increases our perception of pain, and pain can cause insomnia.
“When you can’t sleep well due to pain, this [lack of sleep] leads to more pain,” Dr. Mikhael says. “You also become anxious about not sleeping enough, so you don’t sleep. Then you’re fatigued, so you feel a lot more pain.
“It is a vicious cycle.”
Got a hot tip? Pitch us your story idea, share your expertise with SleepFoundation.org, or let us know about your sleep experiences right here.
It has a wide-ranging impact. Among professions, 86.9% of those employed in manual fields — think farming or warehouse work — reported losing two or more hours of sleep each night to pain, compared to 83.7% in nonmanual fields and 84.4% in tech.
But pain is not reserved only to those in the workforce. Compared to employed individuals, unemployed people, and students, retired people were the most likely (49.6%) to experience pain every night of the week. Retired people, however, also were the least likely to lose more than an hour of sleep to pain each night (75.5%), compared to unemployed people (89.3%) and employed people (84.5%).
What Type of Pain Is Keeping People up at Night?
Pain of all types can prevent people from sleeping. Among survey respondents, 56.2% of people who lost sleep pain experienced back pain, with 41.3% having neck pain, 32.2% having head pain, and 29.4% having knee pain.
When asked to rate their pain on a scale of 0 (lowest pain) to 10 (most severe pain), 73.1% of people say their nightly pain was at level 5 or higher. According to the Mayo Clinic, this means most people surveyed are experiencing at least moderate pain .
What does this all mean?
“Pain does not have to be extreme to keep us awake,” says Dr. Alex Dimitriu, MD, founder of Menlo Park Psychiatry and Sleep Medicine and a SleepFoundation.org medical-review board member. “Even milder forms of pain can result in varying degrees of insomnia, resulting in trouble falling or staying asleep.”
Even when you do fall asleep, sleep may be less restorative when you’re in pain.
“Sleep is as much about quality as it is about quantity,” Dr. Dimitriu says.
“Pain does not have to be extreme to keep us awake,”
— Dr. Alex Dimitriu, Menlo Park Psychiatry and Sleep Medicine
How Has Pain Changed Sleep?
Sleep positions are important. And quite simply, pain in your back, neck, or anywhere else may change how you fall and stay asleep.
You may have to avoid sleeping on your back or side so you don’t put pressure on a certain body part, or you may move from position to position to avoid discomfort.
Drake says his ankle pain makes it difficult to fall asleep many nights.
“When I have ankle swelling, it takes me two to three hours to get to sleep,” he says. “I often wake up with muscle cramps in the night.”
He’s not alone: Among survey participants, 57% of people who experience regular pain wake up at least three times during the night. In fact, it was the top pain-related effect on sleep, with 54.4% of people saying they also have difficulty falling back to sleep after waking. Another 40.9% say they wake up earlier than they’d like. And some people experience all of the above.
This adds up, Dr. Dimitriu explains.
“Falling asleep too late can push circadian rhythms into a delayed sleep-phase cycle,” he says. “And waking too early can result in an advanced sleep phase cycle, where you get tired too early in the evening.”
Irregular sleep patterns can also lead to heightened pain sensitivity, Dr. Dimitriu says, keeping the cycle going.
What Are People Doing To Cope?
Roughly half the surveyed adults, or 54.9%, sought care for their pain from a healthcare professional.
Either way, 69.8% of adults take some sort of medication for their pain, be it prescription drugs (58.9%), nonprescription (53.5%), or a combination of both.
As for the sleeping part: 55.8% of people surveyed who lose sleep to pain have taken sleep aids in the past month alone. Melatonin was the most popular by far, with 49.1% of those respondents choosing it over diphenhydramine/Benadryl (23.4%) and other options.
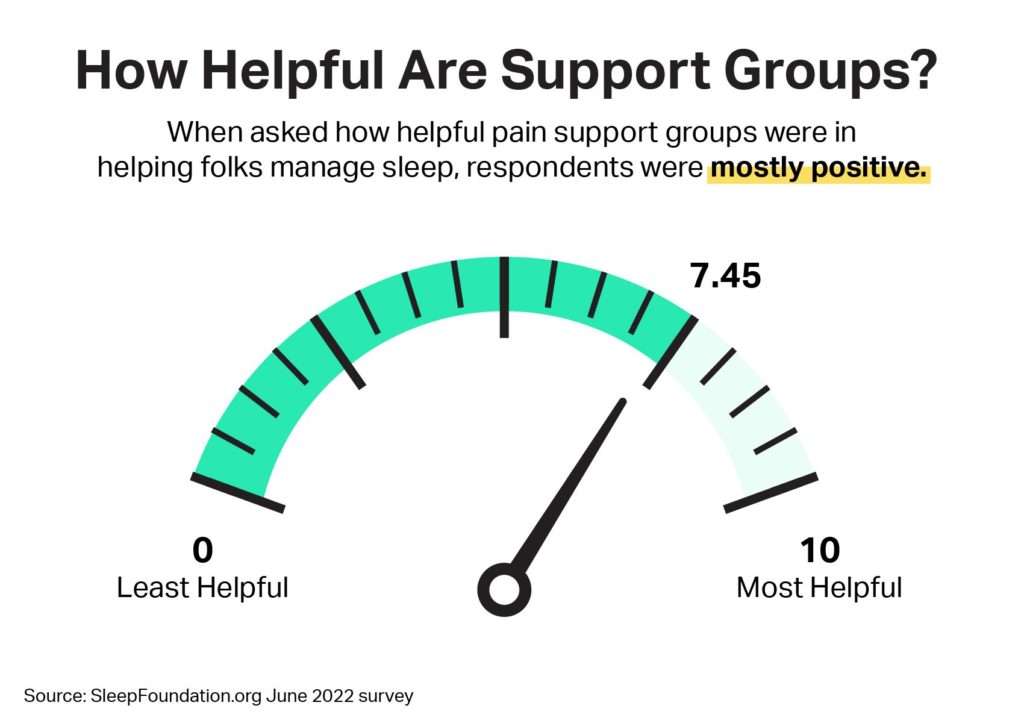
But sometimes, medication alone may not supply results. Support groups — primarily concentrated on social media such as Facebook, Twitter, and Instagram — have emerged to address pain and painsomnia in particular.
Although only 19.5% of people surveyed turned to pain-related support groups, 91.4% say those groups have been effective in helping them manage, understand, or improve their sleep. Many found these groups through simple online searches or via recommendations from health professionals, friends, and family members.
Tonya Coleman Henry, 46, of Central Texas, has turned to online groups for advice about her pain from gastroparesis and migraines, as well as for tips about dealing with insomnia.
“There are many people with many different conditions, but we are all alike in that we experience chronic pain,” she says. “The groups offer a listening ear, compassion, and friendship.”
Women are actually less likely than men to be a member of a support group, with 13.7% taking part versus 26% of men. Meanwhile, access to these groups may be an issue: Only 7.5% for people whose household income is $50,000 or less per year reported using a support group of any kind.
The advice in many of these groups centers on finding strategies for managing pain and sleep. It begins with a mindset that touches on your sleep hygiene, as well, says Ashley Allen, an orthopedic nurse practitioner and CEO of Allen Health & Wellness in Delaware. She recommends checking out Cognitive Behavioral Therapy for Insomnia (CBT-I).
“The idea is that you focus on changing thoughts and behaviors around sleep,” Allen says. “Letting go of the fear of not sleeping is a hugely important step in the process.”
Methodology
This survey was commissioned by SleepFoundation.org and conducted on the online survey platform Pollfish between June 8 and June 9, 2022. Results are from 1,250 survey participants who were ages 18 and older and lived in the United States at the time of the survey. All attested to answering the survey questions truthfully and accurately.
References
8 Sources
-
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., Hazen, N., Herman, J., Katz, E. S., Kheirandish-Gozal, L., Neubauer, D. N., O’Donnell, A. E., Ohayon, M., Peever, J., Rawding, R., Sachdeva, R. C., Setters, B., Vitiello, M. V., Ware, J. C., & Adams Hillard, P. J. (2015). National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40–43.
https://pubmed.ncbi.nlm.nih.gov/29073412/ -
Knutson K. (2015). Sleep and pain: summary of the 2015 Sleep in America Poll. Sleep health, 1(2), 85., Retrieved June 28, 2022, from
https://linkinghub.elsevier.com/retrieve/pii/S2352721815000613 -
Dydyk, A. M. & Conermann, T. (2021, November 11). Chronic pain. In StatPearls. StatPearls Publishing., Retrieved June 27, 2022, from
https://www.ncbi.nlm.nih.gov/books/NBK553030/ -
Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among U.S. adults, 2019. NCHS Data Brief, no 390. Hyattsville, MD: National Center for Health Statistics. 2020., Retrieved June 27, 2022, from
https://www.cdc.gov/nchs/products/databriefs/db390.htm -
Finan, P. H., Goodin, B. R., & Smith, M. T. (2013). The association of sleep and pain: an update and a path forward. The journal of pain : official journal of the American Pain Society, 14(12), 1539–1552., Retrieved June 27, 2022, from
https://pubmed.ncbi.nlm.nih.gov/24290442/ -
Marty, M., Rozenberg, S., Duplan, B., Thomas, P., Duquesnoy, B., Allaert, F., & Section Rachis de la Société Française de Rhumatologie (2008). Quality of sleep in patients with chronic low back pain: a case-control study. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 17(6), 839–844., Retrieved June 27, 2022, from
https://pubmed.ncbi.nlm.nih.gov/18389288/ -
Chang, J. R., Fu, S., Li, X., Li, S. X., Wang, X., Zhou, Z., Pinto, S. M., Samartzis, D., Karppinen, J., & Wong, A. Y. (2022). The differential effects of sleep deprivation on pain perception in individuals with or without chronic pain: A systematic review and meta-analysis. Sleep Medicine Reviews, 101695., Retrieved Oct. 10, 2022, from
https://www.sciencedirect.com/science/article/pii/S1087079222001083 -
Olatoye, Oludare (Dare) O. (2019, June 26). The Dreaded Pain Scale. Mayo Clinic., Retrieved June 27, 2022, from
https://connect.mayoclinic.org/blog/adult-pain-medicine/newsfeed-post/what-to-expect-at-my-pain-medicine-appointment/