Maternity Care Deserts: Home to Sleepless Nights, Exhausted Days

When Katie Archibald was pregnant with her sixth and youngest child in 2021, a 15-minute prenatal appointment “would ruin an entire day.”
There were no OB-GYNs near her home, about 30 miles northeast of Kansas City, Missouri. No hospitals with an obstetrics department. And no family nearby to care for her other five children, all under age 10. So she drove an hour each way to the appointment, plus time spent managing child care.
“By the time I made it home, I was exhausted,” Archibald says.
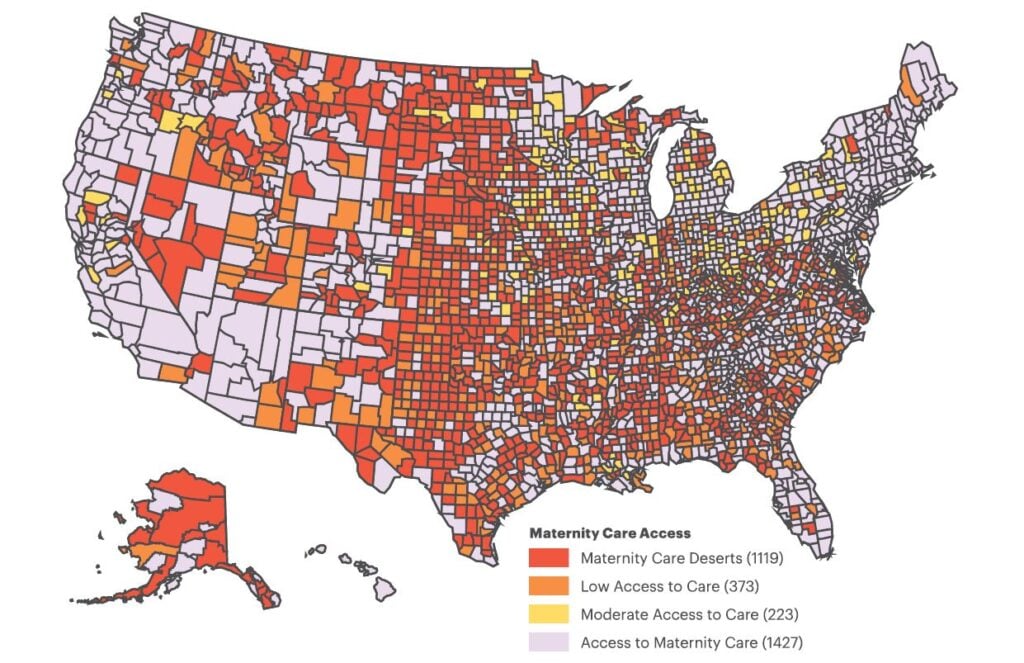
Archibald’s home of Ray County, Missouri , is what the March of Dimes calls a maternity care desert. According to the foundation’s 2022 report on maternity care deserts — which it defines as areas with no pre- or post-pregnancy care, no birth centers, and no OB-GYNs or certified nurse midwives — more than one-third of U.S. counties are in a similar situation. In Missouri, that jumps to 47% of counties, with another 22.6% having “low or moderate care access.”
Nearly two-thirds of maternity care deserts are located in rural areas , with many clustered throughout the South and Midwest. By comparison, California only has five counties (8.6%) that are maternity care deserts. Massachusetts has none.
Got a hot tip? Pitch us your story idea, share your expertise with SleepFoundation.org, or let us know about your sleep experiences right here.
Access to quality prenatal care is critical to maternal health and full-term births of healthy newborns. It’s especially true in terms of getting good sleep during and after pregnancy, from managing the health aspects of pregnancy to the impact that care itself can have on sleep, as in Archibald’s case.
According to an April 2023 SleepFoundation.org survey, female parents of newborns in California and Massachusetts sleep 59 minutes more each night than those in Missouri and neighboring Kansas, where 48.6% of counties are maternity care deserts .
“During prenatal care, health care providers support a pregnant person’s sleep health, identifying and addressing any sleep issues,” says Bilgay Izci Balserak, Ph.D., professor at the Department of Biobehavioral Nursing Science and Center for Sleep and Health Research at the University of Illinois Chicago.
If not treated, a lack of sleep during pregnancy, or sleep disorders such as insomnia, can introduce complications such as preterm labor , gestational diabetes, postpartum depression , hypertension, and low birth weight.
For the 2.2 million women of childbearing age in U.S. maternity care deserts, as well as the nearly 150,000 babies affected, finding a solution to sleep issues and the deficits in care cannot come soon enough.
Care Is Dropping, and Problems May Be Mounting
Sleeping while pregnant is often difficult as it is, says Dr. Nilong Vyas, pediatrician, founder of Sleepless in NOLA in New Orleans, and a SleepFoundation.org medical-review panel member.
“Many changes are happening in the body, and the hormonal shifts responsible for the pregnancy can impact how well-rested a [pregnant person] feels,” she says. “If, during this time, care is not taken to ensure sleep needs are met, it can negatively affect the baby.”
A lack of maternal care raises the risks of pregnancy-related health issues or even death, 80% of which can be preventable , says Terry Plain, a senior strategist with the Missouri Foundation for Health that partners with communities to address inequities in health.
“Less access to maternal care services increases the risk of negative maternal and infant health outcomes,” Plain says. “This is particularly impactful on people of color, where lack of access to care and systemic racial inequities result in Black women and infants dying at rates of up to 3 times that of white women and infants .”
Even as advancements in care itself continue, maternal death rates have steadily climbed among all populations — disproportionately affecting people of color, according to the National Center for Health Statistics .
It’s not just the deaths that are increasing. CBS’ “60 Minutes” recently profiled the prenatal-care issues in Dr. Vyas’ home state of Louisiana, where one-third of parishes are maternity care deserts. Louisiana’s preterm birth rate is 55% higher among Black women than all other women , and female parents of newborns average 5 hours, 45 minutes of sleep a night — far less than the recommendation for any adult — according to SleepFoundation.org’s survey.
Meanwhile, the issues are not necessarily resolving themselves. The March of Dimes report notes that in the past three years, the U.S. has seen a 2% increase in counties classified as maternity care deserts and a 5% increase in those with low or moderate access to care. Rural hospitals’ obstetric-care units are closing at a clip of 9% per decade or faster. And student applications to obstetric programs are down 2% in 2023 from 2022 .
Couple low access or lack of care with needs for specialized care — especially when sleep disorders are involved — and the stakes increase.
Assessing and Addressing Risk
Insomnia is “the most common” sleep issue during pregnancy, Dr. Vyas says. But pregnant people may experience sleep-disordered breathing , ranging from snoring to obstructive sleep apnea (OSA). Restless legs syndrome and pregnancy-related gastroesophageal reflux disorder (GERD) also make it hard to get sleep.
Odds of a preterm birth increase 33.9% when there’s a sleep disorder involved, according to an observational study of California mothers . Considering the same study says 50% of pregnancies include some form of insomnia, with others putting it closer to 100% , it’s a correlation that’s hard to ignore. And it’s where the role of prenatal care becomes clearer.
Tyler Saari, 37, of Buhl, Idaho, turned to her primary care doctor for answers to her sleep troubles while she was pregnant. Twin Falls County, in which her town of 4,500 is located, has one hospital and one OB-GYN group.
A stomach sleeper, Saari found it especially challenging to sleep on her side, which physicians may recommend to improve blood flow . To help, Saari’s physician recommended she take a combination of vitamin B6 and Unisom, which is the brand name of the antihistamine doxylamine.
It was an otherwise uneventful pregnancy. But others in her area drive two hours north to Boise, Idaho, when their pregnancies require specialized care, says Saari, now a nurse herself.
In addition to Archibald’s tiredness on days of her Kansas City appointments, she also says she had trouble falling asleep during pregnancy. She credits that to depression and anxiety, as well as having other young children to care for. Plus, bedtime meant sleeping on her side with a pillow between her knees, two under her head, and one behind her back for comfort — “it was like playing pillow Tetris,” she says.
She ended up taking the antihistamine diphenhydramine, best known by the brand name Benadryl, to help her fall asleep.
“It was the only suggestion I received from my doctors,” she says, “and I was content with that.”
Although Benadryl can make people feel sleepy, its side effects may include daytime tiredness, which Archibald also experienced. Studies also have pointed to its potential negative effect on sleep quality.
Now 41, Archibald also was considered a high-risk pregnancy because she was older than 35 and had gestational diabetes, requiring extra care. In addition to seeing her regular OB-GYN, Archibald had to visit a specialist more than an hour away from home every month. The distance influenced how she felt about the quality of her care.
“I do feel like if my maternal-fetal-medicine specialist were closer, we’d have been able to have better solutions for my gestational diabetes,” she says. “If I had a concern or question they didn’t feel was urgent, I was encouraged just to wait for my next appointment to bring it up.”
Sleep issues or potential disorders can fall into the “miscellaneous” category for many adults, as it may not often come up during conversations with primary care physicians. But during pregnancy, their impact may be amplified. Dr. Vyas, for example, recommends an extra hour or two each night during pregnancy.
Shaving those hours off, as insomnia often does, can be troublesome.
“Insomnia may lead to increased stress, fatigue, and decreased productivity,” Izci Balserak says. “For the baby, maternal insomnia is associated with decreased fetal growth, premature delivery, and low birth weight.”
Improving Access to Maternity Care With Sleep Support
Maternity care in underserved areas still has many challenges to overcome. But there’s hope. The 2022 March of Dimes report calls out Florida, for instance, for making the most improvements to maternity care access, helping more than 92,000 women .
“Promoting preventive, patient-centered, respectful care can provide lasting change and positive impacts,” says Plain, whose Missouri Foundation for Health joins other maternal health stakeholders in supporting regional partnerships, resources, and services to address rural care in particular.
Potential solutions, she says, include mental health screenings, increased training for providers that address respectful care for Black and low-income populations, and home-visit programs. Southeast Missouri’s Bootheel Perinatal Network, for example, helps families access comprehensive care, in addition to addressing food security, transportation, and housing needs.
In Ohio — which the March of Dimes calls out for having the steepest reduction in maternity care — the Bringing Healthy Home supports new parents and families who identify as food insecure or low-income in several counties, including Perry, Jackson, Meigs, and Vinton, all maternity-care deserts.
Community support (or lack thereof) can be another obstacle for those seeking educational classes, breastfeeding support groups, or postpartum care, which includes supporting proper sleep hygiene for new parents. The March of Dimes Mom & Baby Mobile Health Centers aims to address this with services in Washington D.C.; Ohio; the Gulf Coast; and later New York.
More equity-focused initiatives are making moves on Capitol Hill. In 2019, members of Congress created the Black Maternal Health Caucus, which champions legislation such as the Black Maternal Health Momnibus Act of 2021 to address racial disparities in maternal health and aim to increase maternity access for veterans, minority groups, and incarcerated pregnant people.
Telehealth video conferencing also has bridged some gaps where physical care, including sleep support, isn’t available, Izac Balserak says. For example, Dr. Vyas says her New Orleans-based sleep-coaching service works with parents and children throughout the country.
Prenatal care is essential, she says: “It lays the foundation for the baby’s future health.”
Methodology
Data on sleep length for residents of certain states comes from a survey commissioned by SleepFoundation.org and conducted on the online survey platform Pollfish on April 17, 2023. Results are from 1,200 survey participants in the United States who were ages 18 and older at the time of the survey and parent/guardians of at least one child. All respondents attested to answering the survey questions truthfully and accurately.
References
14 Sources
-
Maternity Care Desert Data for Missouri (2022). March of Dimes., Retrieved April 25, 2023, from
https://www.marchofdimes.org/peristats/data?reg=99&top=23&stop=641&lev=1&slev=4&obj=9&sreg=29&creg -
Maternity Care Deserts Report (2022). March of Dimes., Retrieved April 25, 2023, from
https://www.marchofdimes.org/maternity-care-deserts-report -
Maternity Care Desert Data for Kansas (2020). March of Dimes., Retrieved April 25, 2023, from
https://www.marchofdimes.org/peristats/data?top=23&lev=1&stop=641®=99&sreg=20&obj=9&slev=4 -
Vine, T., Brown, G. M., & Frey, B. N. (2022). Melatonin use during pregnancy and lactation: A scoping review of human studies. Revista Brasileira de Psiquiatria (Sao Paulo, Brazil : 1999), 44(3), 342–348.
https://pubmed.ncbi.nlm.nih.gov/34730672 -
Reichner, C.A. (2015). Insomnia and sleep deficiency in pregnancy. Obstetric Medicine., Retrieved May 2, 2023, from
https://journals.sagepub.com/doi/10.1177/1753495X15600572 -
Trost SL, Beauregard J, Njie F, et al. Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 US States, 2017-2019. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2022., Retrieved April 25, 2023, from
https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/data-mmrc.html -
Hoyert DL. Maternal mortality rates in the United States, 2021. NCHS Health E-Stats., Retrieved May 9, 2023, from
https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.htm -
Consensus Conference Panel, Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., Tasali, E., Non-Participating Observers, Twery, M., Croft, J. B., Maher, E., … Heald, J. L. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11(6), 591–592.
https://pubmed.ncbi.nlm.nih.gov/25979105/ -
Hung, P., Henning-Smith, C. E., Casey, M. M., & Kozhimannil, K. B. (2017). Access To Obstetric Services In Rural Counties Still Declining, With 9 Percent Losing Services, 2004-14. Health affairs (Project Hope), 36(9), 1663–1671.
https://pubmed.ncbi.nlm.nih.gov/28874496/ -
Wehrman, J. (2023). OB-GYN workforce shortages could worsen maternal health crisis. Roll Call., Retrieved May 9, 2023, from
https://rollcall.com/2023/03/16/ob-gyn-workforce-shortages-could-worsen-maternal-health-crisis/ -
Izci Balserak, B., & Pien, G. W. (2010). Sleep-disordered breathing and pregnancy: potential mechanisms and evidence for maternal and fetal morbidity. Current opinion in pulmonary medicine, 16(6), 574–582.
https://pubmed.ncbi.nlm.nih.gov/20859210/ -
Felder, J. N., Baer, R. J., Rand, L., Jelliffe-Pawlowski, L. L., & Prather, A. A. (2017). Sleep Disorder Diagnosis During Pregnancy and Risk of Preterm Birth. Obstetrics and gynecology, 130(3), 573–581.
https://pubmed.ncbi.nlm.nih.gov/28796676/ -
Suzuki, S., Dennerstein, L., Greenwood, K. M., Armstrong, S. M., & Satohisa, E. (1994). Sleeping patterns during pregnancy in Japanese women. Journal of psychosomatic obstetrics and gynaecology, 15(1), 19–26.
https://pubmed.ncbi.nlm.nih.gov/8038885/ -
The Manual’s Editorial Staff. (2022, September). Overview of blood. Merck Manual Consumer Version., Retrieved May 9, 2023, from
https://www.merckmanuals.com/home/quick-facts-blood-disorders/biology-of-blood/overview-of-blood









