Epilepsy and Sleep: Understanding the Relationship
Over 3 million people in the U.S. have epilepsy, a brain disorder that involves seizures. Epilepsy can impact people differently, but many with the disorder experience symptoms during sleep. Poor sleep may increase epilepsy symptoms, and people with epilepsy may be more likely to have sleep disorders.
How Epilepsy Impacts the Sleep Stages
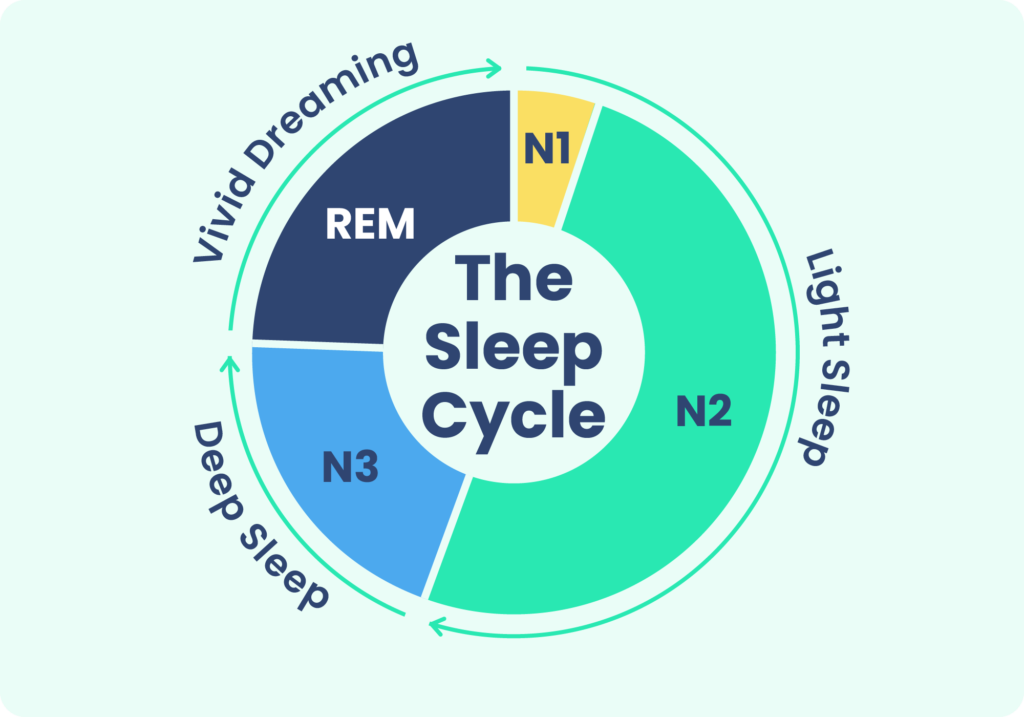
Epilepsy can impact sleep in multiple ways. People with epilepsy tend to take longer to fall asleep and spend more time awake in bed than people without epilepsy. Those with epilepsy also tend to spend more time in light sleep stages and less time in rapid eye movement (REM) sleep, the stage often associated with dreaming, and N3 sleep, the deepest stage of sleep.
People with epilepsy may also experience differences in brain activity during sleep, in the form of a reduced number of sleep spindles. Sleep spindles are patterns of electrical activity seen during sleep that have been associated with learning, memory, and the ability to stay asleep.
The Relationship Between Seizures and Sleep
People with epilepsy can have seizures while asleep, also called nocturnal seizures. Up to 15% of people with epilepsy only have seizures during sleep or immediately after waking. Seizures that occur during sleep are most likely to happen during non-REM sleep stages and are less likely during REM sleep.
Having a seizure, whether while awake or asleep, can further disrupt the sleep of a person with epilepsy.
After a person has a seizure, their sleep architecture can become disturbed. They may sleep much more than normal that night, or for a few nights after. Their sleep may also become more fragmented, even on nights without seizures. They may move through sleep stages more quickly and spend more time awake in bed than usual.
Changes to sleep stages may also be linked to seizures that happen while a person is awake. For example, more time spent in light sleep stages and less time spent in REM sleep could accompany daytime seizures.
If a person experiences a seizure during sleep early in the night, before entering REM sleep, they may spend less time than usual in REM sleep later that night.
The types of epilepsy in which seizures mostly occur during sleep include self-limited epilepsy with centrotemporal spikes (SeLECTS), self-limited epilepsy with autonomic seizures (SeLEAS), sleep-related hypermotor epilepsy (SHE), sleep-related temporal lobe epilepsy, Lennox-Gastaut syndrome (LGS), Landau-Kleffner syndrome (LKS), and more.

Sleep Disorders Linked to Epilepsy
People with epilepsy are more likely to also have sleep disorders. These disorders may include:
- Obstructive sleep apnea (OSA): Between 20% and 40% of adults with epilepsy that doesn’t respond well to medication also have obstructive sleep apnea. When a person has OSA and epilepsy, they may have seizures more often than those without OSA. Treating OSA can help reduce seizures by 50% or more in many of these cases.
- Insomnia: Over half of people with epilepsy have insomnia, which involves daytime tiredness along with trouble falling asleep or staying asleep throughout the night.
- Restless legs syndrome (RLS): RLS causes uncomfortable sensations in the legs, resulting in an urge to move the lower extremities, most often in the evening or while sitting or lying still. In people with epilepsy, RLS is more common and it may contribute to insomnia when a person has trouble falling asleep. Some medications can treat both epilepsy and RLS. Checking iron levels and treating deficiencies may also help.
Epilepsy can also be difficult to distinguish from certain sleep disorders, like REM sleep behavior disorder and parasomnias that occur during non-REM sleep. In these disorders, a person may talk or move during sleep. It is important to discuss these symptoms with a Sleep Physician and sometimes get an overnight sleep study to diagnose the disorder appropriately.
Epilepsy in Children
Children who have epilepsy are more likely to experience sleep troubles than children who do not have the disorder. Epilepsy itself can cause sleep problems, and so can medications children may take for epilepsy. When a child with epilepsy struggles with sleep, they may feel tired during the day, have trouble learning, and have behavioral problems.
Experiencing sleep deprivation may trigger seizures in children with epilepsy, making healthy sleep habits important. If a sleep disorder could be causing poor sleep in a child with epilepsy, experts recommend they undergo an overnight sleep study to investigate as it may impact a child’s social and intellectual development.
Managing Epilepsy: How to Sleep With Peace of Mind
Since sleep and epilepsy impact one another, there are some sleep-related actions people can take that may help with managing epilepsy symptoms.
- Practice healthy sleep habits: Poor sleep can make epilepsy worse, so practicing healthy sleep habits is recommended. Practices that may improve sleep include going to bed and waking up at the same time every day, avoiding caffeine and alcohol in the late afternoon and evening, doing relaxation exercises before sleep, and keeping the bedroom cool, dark, and quiet.
- Review medications: Sometimes sleep troubles or daytime tiredness stem from medications used to treat epilepsy. Looking up potential side effects and discussing current medications with your doctor may help identify factors involved in sleep troubles.
- See a sleep specialist: If a person with epilepsy also experiences symptoms of sleep disorders like obstructive sleep apnea or restless legs syndrome, they should see a sleep specialist. Obstructive sleep apnea is characterized by snoring, daytime tiredness, morning headaches, and other symptoms, while restless legs syndrome involves uncomfortable sensations in the legs.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of sleep health professionals, product specialists, and people just like you. Whether you need expert sleep advice for your insomnia or you’re searching for the perfect mattress, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
5 Sources
-
Lanigar, S., & Bandyopadhyay, S. (2017). Sleep and Epilepsy: A Complex Interplay. Missouri medicine, 114(6), 453–457.
https://pubmed.ncbi.nlm.nih.gov/30228664/ -
St. Louis, E. K., & Foldvary-Schaefer, N. (2023, May 10). Sleep-related epilepsy syndromes. In A.Y. Avidan & P. Garcia (Eds.). UpToDate.
https://www.uptodate.com/contents/sleep-related-epilepsy-syndromes -
Schachter, S. C. (2023, August 3). Comorbidities and complications of epilepsy in adults. In P. Garcia (Ed.). UpToDate.
https://www.uptodate.com/contents/comorbidities-and-complications-of-epilepsy-in-adults -
Moore, J. L., Carvalho, D. Z., St Louis, E. K., & Bazil, C. (2021). Sleep and epilepsy: A focused review of pathophysiology, clinical syndromes, co-morbidities, and therapy. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics, 18(1), 170–180.
https://pubmed.ncbi.nlm.nih.gov/33786803/ -
Wilfong, A. (2023, December 19). Epilepsy in children: Comorbidities, complications, and outcomes. In D.R. Nordli & J.F. Dashe (Eds.). UpToDate.
https://www.uptodate.com/contents/epilepsy-in-children-comorbidities-complications-and-outcomes

































































