Myths and Facts About Sleep
Sleep science has developed significantly in the past 20 years, providing expanded insight about the importance of sleep, the biological mechanisms that control sleep, and the ways it can be disrupted. Despite this advanced knowledge among the scientific community, false information about sleep is commonly spread online or by word-of-mouth. Some of this false information is repeated so often that it becomes a widely held belief, many of which can lead to poor sleep habits and insufficient sleep.
A panel of experts recently identified the most prominent and problematic sleep myths . Getting informed about these myths is an opportunity to gain comprehensive knowledge and find ways to help get the sleep that you need.
Myth: Your body gets used to lack of sleep.
Fact: A lack of sleep takes a toll on your brain and body.
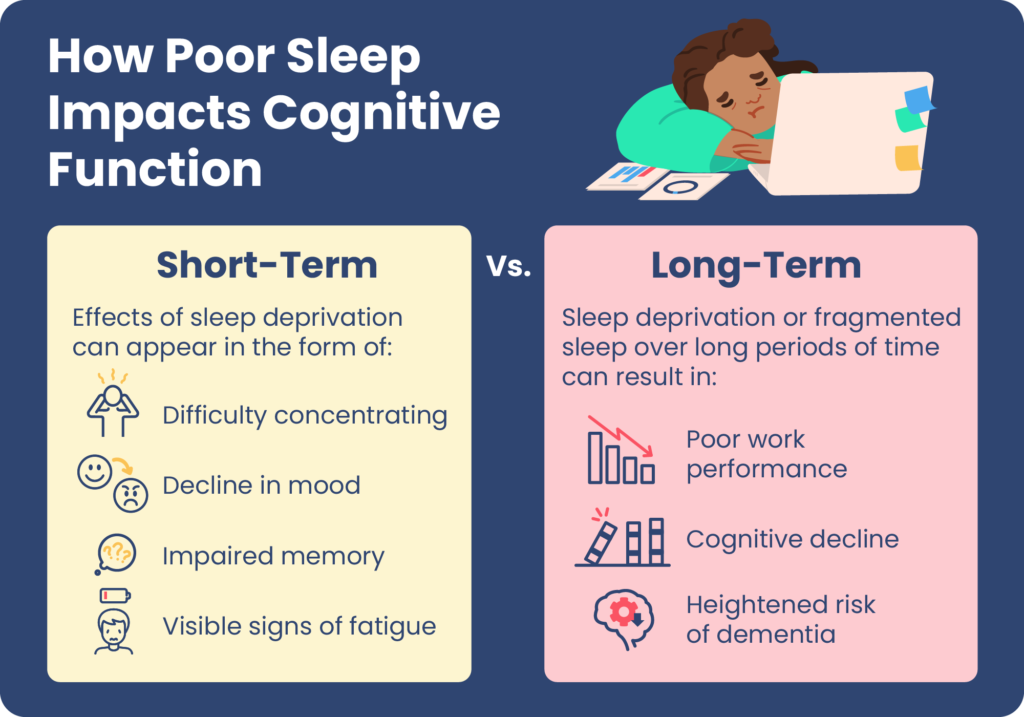
Research has found both short- and long-term negative effects of sleep deprivation, proving that your body does not adapt to lack of sleep.
After a few nights of insufficient sleep, you are likely to feel sleepier during the day. This increase in daytime drowsiness may stabilize over weeks or months without enough sleep, but this does not mean that your body is functioning optimally or is effectively adjusting to sleep loss.
Instead, persistent sleep deprivation affects daytime performance, and can hinder decision-making, memory, focus, and creativity. With time, insufficient sleep can wreak havoc on diverse aspects of health including metabolism, the cardiovascular system, the immune system, hormone production, and mental health.
Even if it seems like you are getting accustomed to sleeping too little, in reality, more serious health problems may be accumulating because of your body’s inability to get the rest it needs.
Myth: How long you sleep is all that matters.
Fact: Sleep quality is another critical factor in sufficient rest.
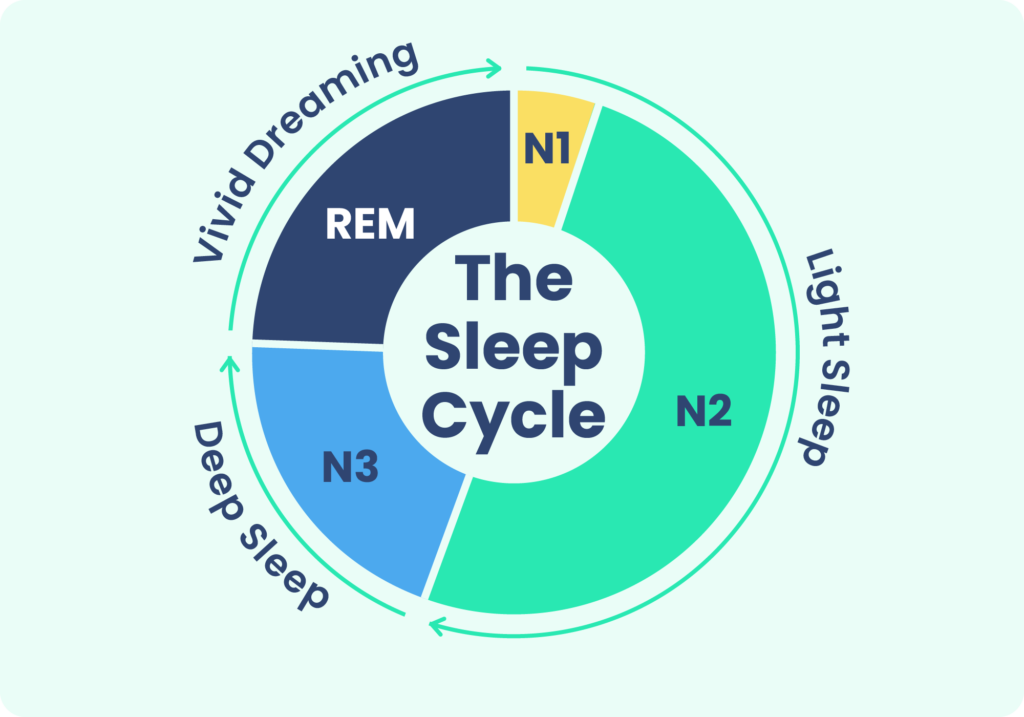
Sleep duration is important, but it is not the end-all, be-all. Sleep quality is another critical factor to consider, and it is closely connected with sleep continuity and lack of sleep disruptions. Fragmented sleep marked by numerous awakenings can interfere with the ability to properly move through the sleep cycle, decreasing time spent in the most restorative stages of sleep. For this reason, every person’s goal should be to sleep enough hours and for those hours to include high-quality, uninterrupted sleep.
Myth: If you are having trouble falling asleep, stay in bed until you can.
Fact: Experts recommend getting out of bed if you have spent 20 minutes trying to fall asleep.
Instead of tossing and turning in bed, it can be better to get up, do something relaxing in a quiet and dim setting such as reading a book – without using your smartphone or other electronic devices – and then try to go back to bed once you begin to feel drowsy.
Experts advise this approach because it is important to associate your bed with sleep. Staying in bed while struggling to sleep can do the exact opposite, linking your bed with a feeling of restlessness.
“Don’t sleep on your sleep problems. Bring up your concerns at your next visit with your health care provider.”
Dr. Abhinav Singh, Sleep Physician
Myth: Alcohol before bed improves sleep.
Fact: Sleep quality declines after drinking alcohol.
A drink or two can be relaxing, inducing drowsiness that makes it easier to initially fall asleep. However, the quality of sleep declines considerably after drinking alcohol, especially in the second half of the night. Consuming alcohol before going to bed can throw off your sleep cycles, make it more likely for your sleep to be interrupted, and may worsen snoring and sleep apnea.
Because of its negative effects on sleep, reducing or eliminating alcohol consumption before bed is recognized as an important part of sleep hygiene.
Myth: A warm bedroom temperature is best for sleeping.
Fact: Most people sleep best in a bedroom around 65 to 68 degrees Fahrenheit.
It is important to find a bedroom temperature that is comfortable for you, but most people find that setting the temperature to mid-60s Fahrenheit is ideal. Although a warm bedroom might feel cozier, studies indicate that it is not conducive to sleep. Body temperature drops naturally as part of the physical process of sleep, and a bedroom that is too hot may disrupt that process. Sleeping hot can be bothersome and interfere with sleep by causing unwanted awakenings.

Myth: Sleeping with a light on is harmless.
Fact: It is best to sleep in a room that is as dark as possible.
Even when you are in bed with your eyes closed, low light can increase the risk of awakenings and may have negative effects on circadian rhythm . Studies have also found that sleeping with too much light in your bedroom can increase eye strain and may be associated with weight gain .
To promote higher-quality sleep and a more stable circadian rhythm, it is best to sleep in a bedroom that is as close to pitch darkness as possible. If reducing ambient light is difficult, consider eyes an eye mask.
Myth: You eat spiders in your sleep.
Fact: People don’t eat spiders while sleeping.
The fear of spiders crawling into people’s mouths at night is widespread, thanks to the internet. However, there is no evidence that spiders willingly crawl into people’s mouths in the night, and it is unlikely that a person would swallow one in their sleep. When spiders encounter a human, they are likely to run away.
Although the myth of eating spiders during sleep is well known, it is not clear how it originated. When researchers who study the spread of misinformation analyzed online news stories about human-spider contact, they found that 43% of stories about spiders were written just to shock the reader. The myth may have also spread quickly since arachnophobia, or fear of spiders, is thought to affect from 2.7% to more than 11% of people .
Myth: Women and men have equal risk of insomnia.
Fact: Women have a lifetime risk of insomnia that is as much as 40% higher than men.
Research shows that women of all ages are more likely to experience poor sleep and frequent instances of sleep disruptions. Some studies point to hormone fluctuation as a potential culprit of insufficient sleep in women, as well as some mood disorders, excessive stress levels, and sleep disorders.
Sleeping problems are also common during pregnancy, with approximately half of pregnant people reporting poor sleep on a regular basis. Women are also less likely to be referred for sleep studies, which can lead to underdiagnosis of potential sleep-disrupting conditions such as obstructive sleep apnea (OSA).
Myth: Napping makes up for a lack of nighttime sleep.
Fact: Naps are not a substitute for quality sleep at night.
While a quick nap can provide a boost of energy during the day, it is not a substitute for quality sleep at night. This is because naps do not involve progression through the stages of sleep in the same way as during nightly sleep.
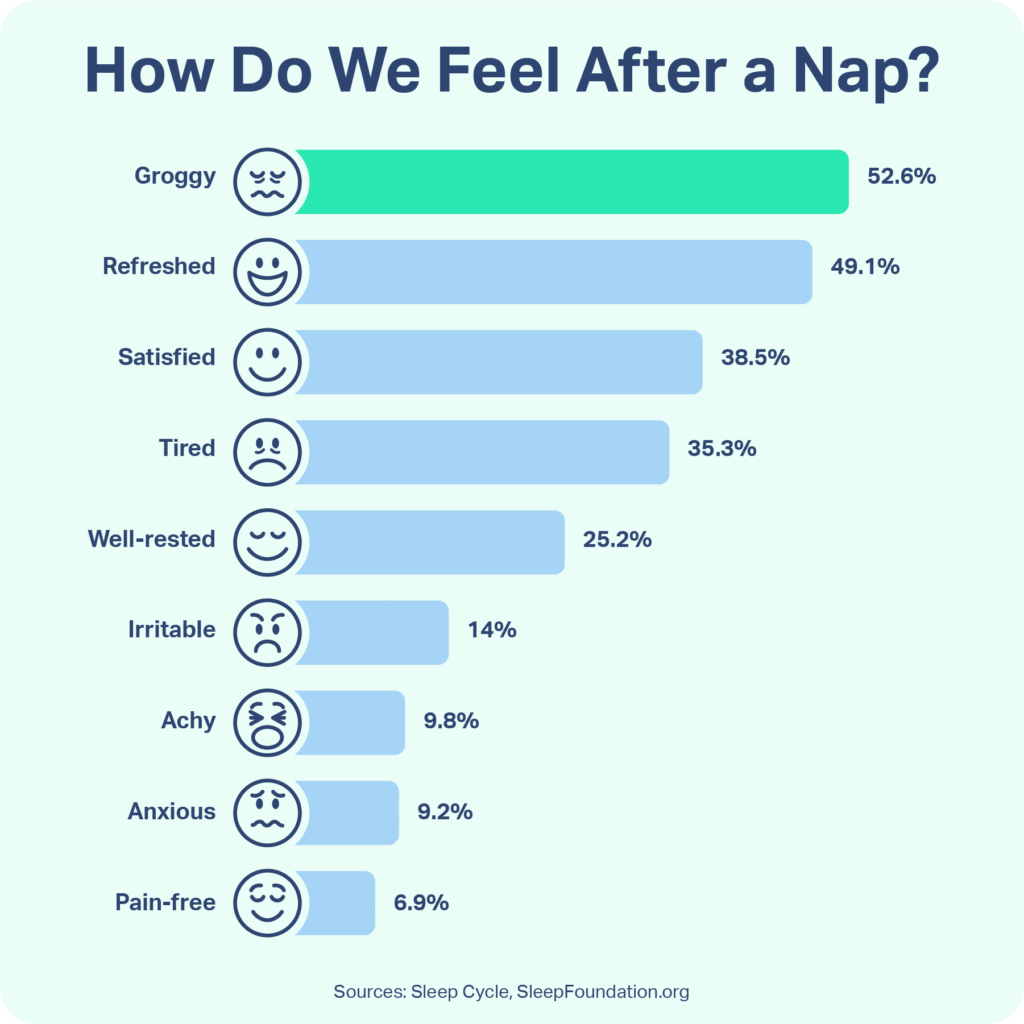
Many people who get insufficient sleep try to use naps to catch up on sleep, but napping can deregulate a person’s sleep schedule even further. Naps can make it harder to fall asleep at a normal time, and long naps can leave you disoriented and sluggish. Though napping is not inherently unhealthy, relying on naps to try to cope with regular sleep deprivation is unhelpful. When you do need a nap, it is best to keep it shorter than 30 minutes and early in the afternoon.
Myth: Snoring is harmless and nothing can be done to reduce it.
Fact: Snoring can be addressed, and severe snoring may be a cause of concern.
Light, occasional snoring is typically not a problem, but loud and frequent snoring may be indicative of some health conditions. If your snoring is loud and frequent, it is important to discuss it with your primary care provider.
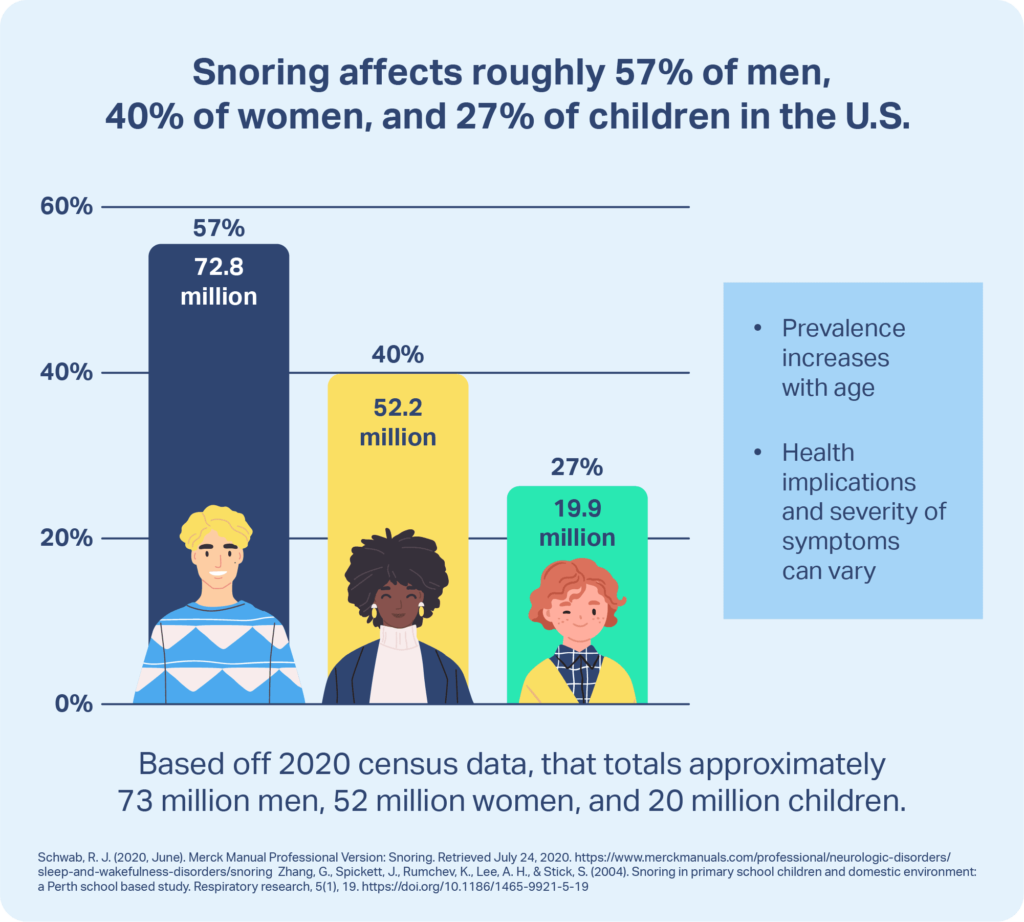
Chronic or loud snoring may be caused by obstructive sleep apnea (OSA), a serious breathing disorder that fragments sleep and prevents a person from taking in the oxygen their body needs. Snoring can also disrupt the sleep of a bed partner or roommate.
Various methods can address snoring depending on its cause. Positive airway pressure (PAP) devices keep the airway open and can help treat OSA. Anti-snoring mouthpieces and mouth exercises can help many people reduce or eliminate snoring, and in some cases, losing excess weight can cut down on snoring as well.

Still have questions? Ask our community!
Join our Sleep Care Community — a trusted hub of product specialists, sleep health professionals, and people just like you. Whether you’re searching for the perfect mattress or need expert sleep advice, we’ve got you covered. Get personalized guidance from the experts who know sleep best.
References
13 Sources
-
Robbins, R., Grandner, M. A., Buxton, O. M., Hale, L., Buysse, D. J., Knutson, K. L., Patel, S. R., Troxel, W. M., Youngstedt, S. D., Czeisler, C. A., & Jean-Louis, G. (2019). Sleep myths: an expert-led study to identify false beliefs about sleep that impinge upon population sleep health practices. Sleep health, 5(4), 409–417.
https://pubmed.ncbi.nlm.nih.gov/31003950/ -
National Institute of Neurological Disorders and Strokes (NINDS). (2023, March 17). Brain basics: Understanding sleep., Retrieved March 27, 2023, from
https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep -
Libman, E., Fichten, C., Creti, L., Conrod, K., Tran, D. L., Grad, R., Jorgensen, M., Amsel, R., Rizzo, D., Baltzan, M., Pavilanis, A., & Bailes, S. (2016). Refreshing Sleep and Sleep Continuity Determine Perceived Sleep Quality. Sleep disorders, 2016, 7170610. https://doi.org/10.1155/2016/7170610
https://pubmed.ncbi.nlm.nih.gov/27413553/ -
Wilckens, K. A., Woo, S. G., Kirk, A. R., Erickson, K. I., & Wheeler, M. E. (2014). Role of sleep continuity and total sleep time in executive function across the adult lifespan. Psychology and aging, 29(3), 658–665.
https://pubmed.ncbi.nlm.nih.gov/25244484/ -
Pietilä, J., Helander, E., Korhonen, I., Myllymäki, T., Kujala, U. M., & Lindholm, H. (2018). Acute Effect of Alcohol Intake on Cardiovascular Autonomic Regulation During the First Hours of Sleep in a Large Real-World Sample of Finnish Employees: Observational Study. JMIR mental health, 5(1), e23.
https://pubmed.ncbi.nlm.nih.gov/29549064/ -
Okamoto-Mizuno, K., & Mizuno, K. (2012). Effects of thermal environment on sleep and circadian rhythm. Journal of Physiological Anthropology, 31(1), 14.
https://pubmed.ncbi.nlm.nih.gov/22738673/ -
Tähkämö, L., Partonen, T., & Pesonen, A. K. (2019). Systematic review of light exposure impact on human circadian rhythm. Chronobiology International, 36(2), 151–170.
https://pubmed.ncbi.nlm.nih.gov/30311830/ -
Suh, Y. W., Na, K. H., Ahn, S. E., & Oh, J. (2018). Effect of Ambient Light Exposure on Ocular Fatigue during Sleep. Journal of Korean medical science, 33(38), e248.
https://pubmed.ncbi.nlm.nih.gov/30224909/ -
Park, Y. M., White, A. J., Jackson, C. L., Weinberg, C. R., & Sandler, D. P. (2019). Association of Exposure to Artificial Light at Night While Sleeping With Risk of Obesity in Women. JAMA internal medicine, 179(8), 1061–1071. Advance online publication.
https://pubmed.ncbi.nlm.nih.gov/31180469/ -
Mammola, S., Malumbres-Olarte, J., Arabesky, V., Barrales-Alcalá, D. A., Barrion-Dupo, A. L., Benamú, M. A., Bird, T. L., Bogomolova, M., Cardoso, P., Chatzaki, M., Cheng, R. C., Chu, T. A., Classen-Rodríguez, L. M., Čupić, I., Dhiya’ulhaq, N. U., Drapeau Picard, A. P., El-Hennawy, H. K., Elverici, M., Fukushima, C. S., … Scott, C. (2022). The global spread of misinformation on spiders. Current Biology, 32(16), R871–R873.
https://pubmed.ncbi.nlm.nih.gov/35998593/ -
Mammola, S., Malumbres-Olarte, J., Arabesky, V., Barrales-Alcalá, D. A., Barrion-Dupo, A. L., Benamú, M. A., Bird, T. L., Bogomolova, M., Cardoso, P., Chatzaki, M., Cheng, R. C., Chu, T. A., Classen-Rodríguez, L. M., Čupić, I., Dhiya’ulhaq, N. U., Drapeau Picard, A. P., El-Hennawy, H. K., Elverici, M., Fukushima, C. S., … Scott, C. (2022). An expert-curated global database of online newspaper articles on spiders and spider bites. Scientific Data, 9(1), 109.
https://pubmed.ncbi.nlm.nih.gov/35347145/ -
Mong, J. A., Cusmano, D. M. (2016). Sex differences in sleep: Impact of biological sex and sex steroids. Philosophical Transactions of the Royal Society, 371(1688).
https://pubmed.ncbi.nlm.nih.gov/26833831/ -
Kızılırmak, A., Timur, S., Kartal, B. (2012). Insomnia in pregnancy and factors related to insomnia. Scientific World Journal, 2012, 197093.
https://pubmed.ncbi.nlm.nih.gov/22623880/